
We take an in-depth look at the for-profit health care in prison and jails in this country. The New York Times published a series titled “Harsh Medicine” based on a yearlong investigation of Prison Health Services, the nation’s largest for-profit provider of prisoner medical care, that exposes how inadequate care has resulted in death and suicides by prisoners. [includes rush transcript]
Today, we are going to take an in-depth look at for-profit health care in prison and jails in this country. Prison Health Services or PHS is the nation’s largest for-profit provider of inmate medical care–a 2 billion dollar a year industry. They have 86 contracts in 28 states and care for 237,000 inmates–which is one in every 10 people who are incarcerated.
Earlier this week, the New York Times published a series, titled “Harsh Medicine.” The articles, based on a yearlong investigation of PHS, expose how the company provided medical care that was widely inadequate in some cases–and deadly in others. The articles detail a range of problems with PHS” medical services–some of which resulted in death or suicides by inmates. The list of problems include: skeletal medical staffs, under qualified doctors and nurses, doctors who were practicing without proper certification, prescription drugs being withheld from patients, and employee misconduct that went unpunished.
PHS began receiving contracts in New York State over the last decade despite a tarnished record of providing care in Florida and Pennsylvania. Since then, the State Commission of Corrections has faulted the company in 23 inmate deaths and has recommended disciplinary action of PHS doctors and nurses, 15 times in the past four years. The New York Times notes that in one report, the chairman of the commission’s medical review board–Frederick C. Lamy–labeled the company, “reckless and unprincipled in its corporate pursuits, irrespective of patient care.” Despite this, New York City renewed PHS’ contract in January of this year.
PHS declined to make someone available for our program but they sent us a statement which reads in part–“since the story appeared, PHS has received calls from clients around the country and every one has been supportive and expressed their disagreement with the Times coverage.”
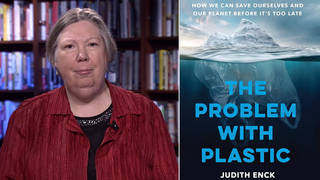
- Paul von Zeilbauer, reporter for the New York Times. Wrote series Harsh medicine about the severe deficiencies of Prison Health Services. PHS is a private company that provides health care to prisons and jails all over the country.
- Dr. Bobby Cohen, federal court appointed doctor who monitors health care in prisons and jails in Michigan, Ohio, Connecticut and New York.
- Barbara Ferguson, sister of Brian Tetrault . Inmate with Parkinson’s disease who, she alleges, was denied proper medical care and died behind bars. PHS was the health care provider in the jail that Brian was locked up in.
Transcript
AMY GOODMAN: Joining us in our studio is Paul von Zeilbauer, the reporter who wrote the series in The New York Times, and Dr. Bobby Cohen, who monitors prison health care for federal courts. On the phone with us from Clearwater, Florida, Barbara Ferguson, whose brother died in a jail cell because he was denied proper treatment by P.H.S. staff, she alleges. We welcome you both and all of you to Democracy Now! Paul von Zeilbauer, this is quite an astounding series. Lay out for us what you exposed.
PAUL VON ZEILBAUER: Okay. Well, over the course of about 15 months, 12 to 15 months, I began looking at the jail medical — the medical — the system of delivering medical care in the New York City jail system where P.H.S. is the medical provider, and there was a series of suicides that occurred in the first half of 2003, and I wrote, I believe, one or two articles, one of which was about how two of these six suicides were people who were on suicide watch at the time, which, you know, brings up the obvious question of what is suicide watch and how does that happen. And from there, we began looking at who the actual provider is, Prison Health Services being the contractor, and then from there, I think it just sort of naturally took a little bit of flight. When you wonder who is doing the medical care, and you begin looking at where else they provide it. And as it turns out, you know, they have had contracts with upstate jails, and of course, they’re a large company, so they have had many other contracts that we just began looking at. And finding other problems, you know, around the country. And that’s how it began, and then, you know, like any good story, the details lead to other details, and you begin opening doors, and that’s how everything sort of came to light over time.
JUAN GONZALEZ: And you originally got on the story because you were covering some of those deaths as part of your regular beat, or how did you get actually involved yourself in the story?
PAUL VON ZEILBAUER: Yes. Right. My job is — in the metropolitan desk at the Times is covering prisons, jails. So Rikers Island was sort of the centerpiece of my beat, if you want to call it that. And so when these suicides occurred, like I said, in the first half — six in the first half of 2001 which may not sound like a lot, but in the world of Rikers Island, it was a lot. In fact, I think I mention in the story, it was the largest — the highest rate of suicide in any six-month period since I think 1985. So, it was remarkable that it occurred, and my beat was covering the jail system and, you know, it became something obviously to look at.
AMY GOODMAN: Tell us about Jose Cruz?
PAUL VON ZEILBAUER: Jose Cruz. Jose Cruz, if I remember correctly, was the first of the six people who killed themselves in this six months period, to do so in January, I believe, of 2003. And, let me see, I don’t want to get any details wrong, but I believe Jose Cruz was a man who was arrested for an assault. He was HIV positive. I believe he had tuberculosis. He was in the — how do you call —- it’s called Maui in the vernacular. How do you refer to -—?
DR. BOBBY COHEN: One of the infirmaries.
PAUL VON ZEILBAUER: Yeah, he was in an infirmary, because he was contagious. And he was also put on suicide watch, because he had become despondent over time. What occurred, if you just want me to give — I can give a quick history of what happened to him. He was put in a cell in this medical lockdown unit that was at the end of the wing where guard — where the jail officers couldn’t visually see him unless they walked down and actually looked into his cell. So, while he was on suicide watch, he was effectively out of sight. And he used that opportunity, apparently, to kill himself.
AMY GOODMAN: I wanted to turn to Barbara Ferguson. If you could tell us the story of your brother. What happened to Brian Tetrault.
BARBARA FERGUSON: Yeah, Brian Tetrault. Good morning. My brother in November of 2001 made the mistake of going to his ex-wife’s house and taking some things he thought belonged to him. She pressed charges and had him arrested. My family and I, who live in Florida, had no knowledge of this at the time. Ten days later, I got a phone call at my house from his ex-wife that my brother died. My brother was very, very sick, very ill. He had undergone some surgeries and things to improve his life, quality of life, but he was an obvious ill person. We were very confused. We had no idea, you know, what had happened. And it wasn’t really until Paul had come to meet with us in last July that I was able to put together the whole story. We didn’t — we were lied to by his ex-wife about how he had gotten into jail. We found out exactly how that happened. But we didn’t understand why he would have died there, and so when we started to pursue some of the information that we wanted, my parents did through the Freedom of Information Act, we got more confused. Just didn’t make sense. Excuse me. As, you know, it got harder and harder to get more information, and also being in Florida, it made it harder for us to try to figure it out. And at one point, my parents tried to be the party to act on my brother’s behalf to, you know, allege a suit against the jail, because we knew that something had happened, and in that pursuit, my nephew was named the person who would do that, and he is in the suit with them currently.
AMY GOODMAN: When we come back from our break, we’ll find out more about the circumstances of when he was put into jail. Our guest, Barbara Ferguson, who lost her brother in the New York City jail system — the New York State jail system. Dr. Bobby Cohen, who is the federal court appointed doctor who monitors health care in the prisons, and Paul Von Zeilbauer, who is the reporter for The New York Times that did this series for The New York Times called “Harsh Treatment.”
[break]
AMY GOODMAN: We’re talking about “Harsh Medicine.” It’s a series of exposés in The New York Times this week by Paul von Zeilbauer about the Prison Health Service, which is P.H.S., a for-profit prison health care industry in this country. And we’re looking at some of the cases he exposed this week. We’re also joined by Bobby Cohen, who is the federal monitor for prisons, as well as Barbara Ferguson, who has been telling us the story of her brother, Brian Tetrault, who died in his jail cell. I’m Amy Goodman here with Juan Gonzalez.
JUAN GONZALEZ: Paul, let’s continue with the Brian Tetrault case. Again, how did you get on this particular case? He was a former nuclear scientist who had struggled with Parkinson’s disease and was in jail on a minor charge.
PAUL VON ZEILBAUER: How I got onto that —
JUAN GONZALEZ: And also, then, what you discovered about his case.
PAUL VON ZEILBAUER: As I mentioned to you, after I began looking at the — after the company’s record became an issue and became relevant, I went to the State Commission of Correction. It’s a small agency in New York State. Its members are appointed by the Governor, and its mission is to enforce standards in the New York City jails — sorry, in the jails and prisons in New York State. It actually — this Commission began as or got its current mandate after the Attica riots, I believe, in 1971, to prevent that very thing from happening again and to make sure there were humane levels of care and so forth in the jails and prisons. So, what the Commission does is investigate every jail death that occurs, whether it’s in a, you know, Broome County jail or whether it’s in Attica or another state prison. So, they publish these reports. The reports are public. I filed a Freedom of Information Act request for every report that the Commission had done that mentioned or included or referred to Prison Health Services, because like I said, the company had become a focus of my reporting. So, Mr. Tetrault’s case became — was one of those reports. In fact, it’s interesting, you know, there were many reports that I received. Some were more interesting than others. And Mr. Tetrault’s case was interesting because he had died in 2001, but the Commission Of Correction only became aware of his death in 2003, by mistake, really. One of their employees read a newspaper article upstate that explained one of his family members had filed a lawsuit over the death, which was news to the Commission. And so they began looking into it and found, you know, this case.
AMY GOODMAN: So in that particular case, the correctional authorities had not reported the death to the Commission?
PAUL VON ZEILBAUER: Yeah. It was the Schenectady County Jail where Brian Tetrault was incarcerated. And the law in New York says that every time you have a death of an inmate, every time an inmate dies or is injured, you have to —- excuse me -—
AMY GOODMAN: Turn off your watch?
PAUL VON ZEILBAUER: Yeah, turn off your watch and then report it to — no, you have to report it to the State Commission, so that there is no excuse for not having a public inquiry. But in this case, Brian Tetrault was released — was supposedly released from jail, even though he was in the hospital bed by the time he died. He was released by the sheriff’s office ten minutes before, supposedly ten minutes before he expired.
AMY GOODMAN: I want to just read those first two paragraphs of your piece, “Private Health Care in Jails Can Be a Death Sentence.” “Brian Tetrault was 44 when he was led into a dim county jail cell upstate New York in 2001, charged with taking some skis and other items from his ex-wife’s home. A former nuclear scientist, who’d struggled with Parkinson’s, he began to die almost immediately, and state investigators would later discover why. The jail’s Medical Director had cut off all but a few of the 32 pills he needed each day to quell his tremors. Over the next ten days, Mr. Tetrault slid into a stupor, soaked in his own sweat and urine, but he never saw a jail doctor again, and the nurses dismissed him as a faker. After his heart finally stopped, investigators said corrections officers at the Schenectady jail doctored records to make it appear he had been released before he died.” Dr. Bobby Cohen, how did this happen?
DR. BOBBY COHEN: Well, I think that the problem in medical care in prisons is that for a variety of reasons — and this is a general issue, not specifically on what Paul wrote — is that medical care operates within prisons and tends to see its role as supporting its client, which is the system, which is the jail, which is the city, which is the state, rather than the patient. Now, that’s not always the case. There are dedicated people, and you know, Paul’s article talked about people who had really tried to do a good job. But the nature of incarceration creates a very, very difficult situation in which to provide medical care. It’s possible, but difficult. And it is deforming to medical staff just as it’s deforming to prisoners and to correctional officers to be in these institutions, but it’s hard to understand how nurses could ignore a situation that was just described right now, or how doctors could ignore a situation that — like that, which was described. That is incredibly disturbing, and it happens. It’s not the usual, but it happens. It happens often enough. I think that the task is to — in terms of providing medical care in prisons — is to instill and inspire medical staff to understand that their job is difficult, and it can only be done in opposition, actually, to the prison. You cannot provide medical care in a prison, if you go along with the prison rules. You have to complain when patients are not seen. You have to complain when transportation doesn’t bring the patient to the specialist. You have to complain when medications are not delivered. Now, I think it is particularly hard for for-profit companies to do that, because they need to have their contract renewed by the facility or the state or the county, and they want to be on good terms with them and not make their job of corrections more difficult.
JUAN GONZALEZ: Well, but Paul, I’d like to ask you, I remember years ago, I covered quite a bit of what was going on in the city jails at The Daily News, and I would often get calls from doctors or medical staff who worked on Rikers Island. At that time it was Montefiore Medical Center which had the contract. It was a non-profit voluntary hospital in New York to handle the situation and to deal — provide medical treatment to Rikers. But there would be doctors and nurses who were definitely concerned about what was going on and the kind of treatment that they were being forced to deliver. What has been, from what you can tell, the impact of this move toward more for-profit operations moving into these jails?
PAUL VON ZEILBAUER: Well, in the — I can speak in the context of what I have learned through my reporting, and what I understand is that privatization of — if you want to call it private, I mean, it’s a public company, Prison Health Services, so “private” is a bit of a misnomer, but it seems as if the difference between a for-profit company providing jail or prison health care and a teaching hospital or a public hospital doing it is that the staffs — the staffs, the clinical staff seems to be smaller. I mean, that just seems — not just in New York City that it occurred, but it’s what I found everywhere.
AMY GOODMAN: You used the term “skeletal.”
PAUL VON ZEILBAUER: Yes, the doctors used that term. In fact, I think it was the first article of the three here quoted a doctor who had just resigned in Alabama. She was one of, I think, two doctors in the prison, the state prison in Alabama for about 2,200 inmates who had complained about absolute skeletal staff. This is — I mean, the reason we used it not because it was an aberration or a nice word it use to play gotcha, but it really reflected what I had heard from medical clinicians and medical people who worked for this company in many places.
AMY GOODMAN: A second story in your piece. You say, “Two months later, after Mr. Tetrault died, Victoria William Smith, mother of a teenage boy was booked into another upstate jail in Duchess County, charged with smuggling drugs to her husband in prison. She, too, had only ten days to live after she began complaining of chest pains. She phoned friends in desperation. The medical director would not prescribe anything more potent than Ben Gay or the arthritis medicine she had brought with her, investigators said. A nurse scorned her pleas to be hospitalized as a ploy to get drugs. When at last an ambulance was called, Ms. Smith was on the floor of her cell shaking from a heart attack that would kill her within an hour. She was 35.” Now, Dr. Bobby Cohen, you’re the Federal Court appointed doctor who monitors health care in prisons and jails in Michigan, Ohio, Connecticut, New York. Where does P.H.S. fit into this? Prison Health Services. How does it compare to non-profits that run the system. We’re sorry they couldn’t be us with, but is this a serious crisis in this country, and should they have their contracts pulled?
DR. BOBBY COHEN: I have not had a chance to review all of the data that Paul looked at, although I have no reason to believe that he did not carefully review it and that it reflects the reality. Certainly, New York City should have thought very carefully about renewing it at that time, and there should have been a process which allowed this information to get out. I think that in general, the trend towards for-profit health care in the United States is a serious problem, that just as in other health care in the United States, when you put profit into the situation, you get that profit significantly by denying care. And when a company like P.H.S. or other for-profit companies go into a system, the first thing they establish is a utilization review system, which all of your viewers are familiar with from their own encounters with medical care. Utilization review is a really a process of denying access to specialty care. That’s in a contract where there’s a fixed amount of money, and whatever they don’t spend, they keep. That’s a very easy way and effective way to make money. That was not the case on Rikers Island right now, because the previous contractor had had a risk contract where they made millions and millions of dollars, tens of millions of dollars by denying care on Rikers Island. Actually, they were kicked out because of the serious morbidity and mortality, many, many deaths that occurred during the St. Barnibace reign. I think that there is no room for for-profit health care in prisons, because of the kinds of situation that Paul has described. The process, when a company goes in, and then it gets its contract renewed after two or three years, it essentially has to underbid itself because there are other for-profits who are willing to come in and take the care, so it doesn’t ask for increases in fees. When I monitored the Philadelphia jails a number of years ago when P.H.S. was running it, I encouraged them to ask for additional funds when they were renewing the contract, because they had new problems. They had to take care of HIV infection. They had to fix what was not being done. And they were extremely reluctant to do that, because they knew that they would lose their contract. And so this — the process of competition among for-profits drives the amount of funds available to prisoners down. And that’s a serious problem.
JUAN GONZALEZ: Doesn’t ultimately the problem reside in the fact that, because we are dealing with an inmate population or prisoner population that the local governments, the state governments basically don’t care, and want to spend as little money as possible in maintaining the health of these inmates, and there is no constituency — organized constituency to insist on better health care?
DR. BOBBY COHEN: I think that’s absolutely right, and it actually is the law in this country. I mean, there are two legal issues. One, in the United States, prisoners are actually entitled to health care which is not deliberately indifferent to their serious needs. The Supreme Court ruled that in 1976, and that’s why all of the lawsuits have been filed, and actually, P.H.S. exists because of these lawsuits, because they said, “We can fix it,” when the courts told the states or the cities that you are providing unconstitutional care. But there’s another legal issue here, which is that the cities and states cannot say it’s P.H.S.'s fault. They are responsible. And they have to monitor it. As Paul points out in the article, previously, New York City's Board of Correction, which developed standards for care of medical and mental health in the jails, had a death review board, which reviewed every death, and that process has not been continuing of late. More of that is needed. More involvement of —- you know, I really think the more non—— the more people who come into prisons and see what’s going on, the more people looking the better, because these are deforming, terrible institutions that need as much fresh air as possible.
AMY GOODMAN: Tell us about the Philadelphia case that you’re quoted in the article, Dr. Robert Cohen, about women who were pregnant in the Philadelphia jails. Again, this Prison Health Services provides service in this case. “In Philadelphia in 1999, federal court monitors report warned the company’s failure to segregate prisoners who were suffering from T.B. posed a public health emergency. Pregnant inmates, it said, were not routinely tested or counseled for HIV, endangering their babies. In fact, the women were encouraged to refuse pelvic exams.”
DR. BOBBY COHEN: I believe that I was the state monitor at that time. There’s another doctor, Robert Greifinger, who was the federal monitor at that time. My experience in Philadelphia, in terms of care for women in prison, was that there was a process in which women were encouraged to refuse pap tests and pelvic examinations. I would look at the charts and they would say, “refuse, refuse, refuse, refuse, refuse.” And then I would ask people, and they told me why, that there were — when supposedly these exams had taken place and they were tested for chlamydia or gonorrhea, common illnesses among women who were in prison, the rates were unbelievably low to zero when we know that the rates of these are very, very high in this population. Additionally, while I was there, while I was reviewing it, two women delivered in their cells who were pregnant. That’s — there’s — of course, these things happen, but it’s usually a story in The Daily News, when someone delivers in a cab. This does not have to happen in a setting with medical care present.
JUAN GONZALEZ: Paul, I’d like to ask you, who runs P.H.S.? Who are the — I mean, there are obviously individuals behind these companies. Is it part of a larger corporation, and how did it develop?
PAUL VON ZEILBAUER: Yeah, well, Prison Health Services was founded in 1978, not coincidentally, I believe, two years after the Supreme Court ruling that Dr. Cohen mentioned that required adequate medical care to be provided to all inmates. So, you know, there was an opportunity there, because governments weren’t interested in it, and in providing it necessarily. I mean, they had to, but they weren’t eager to. Companies like Prison Health evolved, and currently the company — make sure I get this right, Prison Health Services is a — there’s a holding company that basically owns Prison Health Services. The holding company is called America Service Group. Its stock ticker is A.S.G.R. It’s based in Tennessee. Under the America Service Group umbrella, there is Prison Health Services, and there is a pharmacy operation called Secure Pharmacy Plus, which, you know, is a complementary business because the pharmacy provides the medicines to the jails and prisons where P.H.S., Prison Health Services has contracts. So, it — you know, the — it’s a public corporation. You can go on the S.E.C. website or anywhere else — or your Ameritrade account, for that matter, and look up the company’s performance and who owns it. It’s a regular public company.
AMY GOODMAN: Just ending with Barbara Ferguson. What are you calling for right now in the death of your brother?
BARBARA FERGUSON: At this point, my family, meaning myself and my parents, we are not doing any legal action. My nephew is doing that. He, I believe, and Paul, you can verify this, because you probably have more information. They are trying to settle a suit, I believe, with Prison Health Services. But what we really, really want is that, to go along with Paul, to help these people be aware.
PAUL VON ZEILBAUER: This, I mean, as Dr. Cohen mentioned, it’s just — you know when you go into jails and prisons, it’s by almost necessity, but certainly, there is not a lot of sunlight shed on these institutions.
AMY GOODMAN: Well, thank you for doing some of that with your series, “Harsh Medicine.” I want to thank you, Paul von Zeilbauer for joining us, reporter for The New York Times, wrote the series in the paper.
PAUL VON ZEILBAUER: Sure.
AMY GOODMAN: Dr. Robert Cohen, federal court-appointed doctor, who monitors health care in prisons and jails, and Barbara Ferguson, sister of Brian Tetrault, who is the prisoner with Parkinson’s who, denied proper medical care, died behind bars.











Media Options