
Related
Guests
- Uché Blackstockemergency medicine physician, author and founder of Advancing Health Equity.
Part 2 of our conversation with Dr. Uché Blackstock about her new book, Legacy: A Black Physician Reckons with Racism in Medicine.
Transcript
AMY GOODMAN: This is Democracy Now!, democracynow.org, The War and Peace Report. I’m Amy Goodman, with Nermeen Shaikh.
This is the first day of Black History Month. We’re talking to Dr. Uché Blackstock, Part 2 of our conversation with the emergency medicine physician, CEO and founder of Advancing Health Equity, a company that works with healthcare organizations to fight racism and bias in services. Dr. Blackstock has written a new book. It’s called Legacy: A Black Physician Reckons with Racism in Medicine.
You know, Dr. Blackstock, I wanted to go back to, really, the beginning of our Part 1 conversation, but to really give you time to tease out your life story, your mother this pioneering Black woman physician, who dies at such a young age, gives birth to you and Oni, to Dr. Oni and Uché Blackstock —
DR. UCHÉ BLACKSTOCK: Yes, yes, yes.
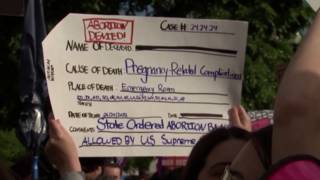
AMY GOODMAN: — following in her footsteps — and all the issues that you took on through the years. One of the things you talk about in Legacy is the fact that 2% of America’s doctors are African American women, just 2%. And yet the mortality rate, for example, just when it comes to Black maternal health, is so disproportionate.
DR. UCHÉ BLACKSTOCK: Yes. So, yeah, so I’m happy to talk a little bit about my mother. You know, when I was younger, I thought that all physicians were Black, or Black women. Like, that’s the kind of exposure that I had with my mother.
So, she was born in central Brooklyn to a single mom. My mother had five other siblings, and they were raised on public assistance. They had a very, very difficult life, moving a lot, food insecurity, changing schools. But my mother, you know, she was very, very, very determined. She was very intellectually curious. And she was fortunate enough to end up at Brooklyn College and had a chemistry professor there who saw her lights or her potential — a Black man — and said, “You know, you should apply to medical school.” So she ended up applying to medical school and ended up being accepted to all of her medical schools and matriculated at Harvard Medical School, where, obviously, she felt like a fish out of water. You know, she was in school with students whose parents had written the textbooks that they were using. Another student’s parent had won the Nobel Prize in immunology. But she found her group of friends there, and she was able to make it through.
And what really strikes me about my mom is that she could have gone anywhere after Harvard Medical School, but she came back to New York City, trained at Harlem Hospital, and then worked in the same neighborhood that she grew up in, at SUNY Downstate/Kings County Hospital, as a nephrologist, as a kidney doctor, and worked with, you know, other Black women physicians and held community health fairs and diabetes screenings, connecting patients to social services. So, I write in Legacy that my mother was practicing what’s now known as structurally competent and culturally responsive care, where she really saw and understood the social and political context in which her patients were living. You know, I think a lot of times in medical school we’re taught that, you know, what physicians do is just, you know, we prescribe medications, tell people to eat healthy. But my mother understood, when she was in the room with her patients, that she wasn’t just in the room with them; she was in the room with their family members, their co-workers, all of their loved ones, and all of the factors that impact how healthy they are.
And so, my sister and I, today, we both have our own health equity consultancy firms, working with healthcare organizations to dismantle racism in medicine, but we are continuing her legacy, this legacy of working in service to Black communities. We know that today racial health inequities are actually worse than they were in the ’80s and ’90s. Maternal mortality is actually getting worse. And so, I think that just shows how deeply embedded racism is, not just within healthcare, but within all of our social systems.
AMY GOODMAN: Your mother died of leukemia in her forties?
DR. UCHÉ BLACKSTOCK: Yes. And she was — my mother was full of life. She ran every day, took great care of herself. And we actually ran a race together in Central Park about a few months before she was diagnosed. And even though my mother, you know, was was in her forties, she was faster than my sister and me, who were 18 years old. And she came in after us, and we said, “Mommy, are you OK?” And she said, “I’m just really tired.” A few months later, she was diagnosed with acute myelogenous leukemia and, unfortunately, was given a very poor prognosis.
During the workup, we took her to Dana-Farber Institute, and which — in Boston, you know, cancer specialty center. And the doctor said, “It looks like you were exposed to radiation, like the way that your chromosomes look.” And so, you know, in doing the research for this book and talking to other oncologists, it’s quite possible. You know, my mother grew up in a lot of neighborhoods in Brooklyn that were Superfund sites that had toxic dumping. So it’s very likely that she could have been exposed to radiation in her communities because of environmental racism, growing up.
But, obviously, for my sister and me, losing our mother at 19 years old, it was like the rug being pulled out from underneath us. But she has still had a profound impact on the work that we do today.
NERMEEN SHAIKH: So, Dr. Blackstock, if you could talk about that, the way in which you and your sister have kind of followed your mother’s example? Talk about your journey, where you started out and the work that you’re doing now, the importance to you of this organization, Advancing Health Equity.
DR. UCHÉ BLACKSTOCK: Yes. And so, what I would say is, you know, I’ve been on my own journey, from child to medical student to practicing physicians and — practicing physician. And it really is as a practicing physician that I recognize the gaps in the education and training that I received. It wasn’t until I was in my residency program in emergency medicine at Kings County/SUNY Downstate, public hospital and state-run hospital, that I began to recognize the impact of social determinants of health, like education, employment, you know, housing, on my patients’ health.
I ended up going into academic medicine, which is what, you know, a small percentage of all physicians go into. It’s supposed to be very prestigious. It was something — you know, my mother also was in academic medicine. And I think what I found in that environment — you know, I was at NYU School of Medicine. I was the only — at times, one of the only Black faculty members in my department. And this is in the middle of the most diverse — one of the most diverse cities in our country. But I was very isolated. I didn’t receive a lot of mentorship. I was actually appointed to a diversity, equity and inclusion role within the medical school, was very excited about that, and soon found out it was just a figurehead role and that I really couldn’t do the work around health equity and diversity, equity and inclusion authentically. And it became very clear to me soon that I would have to leave that institution in order to be really in alignment with doing the work that I wanted to do, and that, you know, to be honest with you, a lot of academic medical centers and higher education, these environments are not very inclusive of Black faculty or Black students. So I made the decision to leave.
I founded Advancing Health Equity. It’ll be five years old in March, next month. And I’m able to do the work that I’ve always wanted to do. We work with healthcare organizations, hospitals, public health agencies, around creating diverse, inclusive workplaces and also providing the opportunity to provide racially competent care to our patients. So we do equity assessments, program evaluations, leadership coaching. And so, it’s my way of making an impact. When I left academic medicine, I felt very guilty about leaving our students behind, our Black students especially, because I know that they have very few mentors. But what I recognized was that by actually leaving, I was showing them there was a different journey, a different path that you can take, to make an impact to work in service to our communities.
AMY GOODMAN: Dr. Uché Blackstock, in Part 1 of our conversation, you referenced weathering. Can you go more deeply into this concept?
DR. UCHÉ BLACKSTOCK: Yes. You know, so, I think it’s really important for people to understand, like, the myriad of ways that racism, interpersonal and systemic, impacts Black health. And so, the public health researcher Arline Geronimus, she coined this term, where she was actually studying, you know, pregnant — birthing people and noticing that birthing people of color were more likely to have, you know, complications or deliver their babies early, and really came up with this concept that, you know, dealing with any kind of stress, whether it is growing up in poverty, whether it is dealing with racism, over time, it wears down the body. It’s a chronic wear and tear, and it prematurely ages the body so that it makes Black people more susceptible to developing different diseases. So, for example, you know, we know that Black people often carry a higher burden of diabetes or high blood pressure, asthma. You know, this is not because there is a gene in us that predisposes us to this, but this is actually the impact of chronic stress on our body that makes it more susceptible to developing these chronic diseases.
Another thing I just wanted to mention is this idea of epigenetics, which is really — has been well studied, but it’s this idea that the stress of racism actually changes gene expression, so that we know that Black people are more likely to have autoimmune diseases, diabetes, heart disease. And that’s another kind of example of how stress, the stress of just living with everyday racism, poorly impacts our health.
AMY GOODMAN: You worked at NYU Medical School, which is now free. What kind of difference do you think that will make? And I want to go from medical school — I mean, it’s interesting, because NYU is one of the most expensive universities in the country.
DR. UCHÉ BLACKSTOCK: Right.
AMY GOODMAN: But also then going to the issue of universal healthcare, of healthcare for all, and the kind of system that we have in this country and how it affects communities of color.
DR. UCHÉ BLACKSTOCK: OK. So, I will say that, you know — I’m going be honest, very transparent. The new program or the new system that NYU has, where it is tuition-free, I think, on the surface, looks, you know, amazing as an opportunity for equity. However, you know, I don’t think they’re taking into consideration people’s, like, socioeconomic status, people’s backgrounds. I think they’re still very much looking at GPA and MCAT scores. And so, what I think is really important is for, in the admissions process, if we are going to have tuition-free programs or provide students with grants so they don’t have to take out scholarships, I think we need to take into — it needs to be an equitable system. You know, if people are coming from families with generational wealth, I don’t think they necessarily need to benefit from a tuition-free system. However, if they are coming from families that have lacked generational wealth, you know, for generations, then that seems more appropriate to me. So, I am more for systems that are going to take into consideration a student’s background, racial and socioeconomic status, in making decisions about who goes to school tuition-free or not. So, that’s one thing.
I do think that it is important to think about how do we incentivize our medical students to go into primary care or other areas, like primary pediatrics, geriatrics, specialties that are not what we call well compensated compared to other subspecialties, like plastic surgery or dermatology. There is a dearth of primary care physicians. And part of that reason is because medical students are leaving medical school with these, you know, high loan burdens. And then, you know, they’re thinking, “OK, that means I have to go into a specialty that pays well.” And so, I think it’s really up to medical schools, academic medical institutions, and our local, state, federal government to think about ways, you know, where people don’t — where students don’t have to take out loans, where they say, “I’m going to work in underserved communities.” And that makes more sense for me to incentivize for a tuition-free program.
AMY GOODMAN: And what about universal healthcare, healthcare for all?
DR. UCHÉ BLACKSTOCK: Oh, absolutely. You know, I write about this in Legacy. As you mentioned earlier, you know, we’re one of the only high-income — we are the only high-income country, we have the worst health outcomes, and we don’t have universal healthcare. I personally advocate for a single-payer, universal healthcare, because we know, you know, when we look at the calculations and statistics, not only would we save tremendous amount of money, but we would save a tremendous amount of lives. We know that in states that have had Medicaid expansions, that people do better. There are better health outcomes. So, those 10 or 11 states that have not expanded Medicaid, people in those states are suffering.
So, you know, one of the things that I write about in this book is, really, the importance of healthcare as a human right. And also, I think it’s a racial justice issue, as well, because we know, of the uninsured in this country, the majority of them are people of color. So, I do think that, you know, I’m all for a Medicare for All. You know, right now this decentralized, fragmented, for-profit healthcare system that we have, it obviously is not working. If it was working, you know, we wouldn’t have the highest overdose rates. We wouldn’t have the highest maternal mortality rate. We wouldn’t have the highest suicide rates. You know, our system is very, very broken. And I really would love for our policymakers to be brave and, you know, consider the importance of single-payer, universal healthcare.
NERMEEN SHAIKH: Dr. Blackstock, if you could elaborate on this point of universal healthcare, when it comes, in particular, to the conversation with which we started, which is about maternal mortality rates here? Because giving birth in the U.S., on average, costs $18,865. That includes pregnancy, delivery and postpartum care, this according to the Peterson-Kaiser Family Foundation Health System Tracker. Almost $20,000.
DR. UCHÉ BLACKSTOCK: Yes. And, you know, I write about this in my book, that there is a reason for this. You know, there was an act called, I think, the Sheppard-[Towner] Act in the early 1900s, which essentially did away with or erased midwives, essentially, made — there was a public health campaign that made having midwives seem like unsanitary, associating them with poor health outcomes. And essentially, what that did was it medicalized the birthing process. So, it essentially elevated the role of physicians, obstetrics-gynecologists in the birthing process. And as a result of that, you know, over time, that has actually led to more in-hospital deliveries.
So, that’s the other reason why birthing in this country is so expensive, is that there are so many — the majority of people give birth in a hospital. And there are financial, obviously, incentives for that. You know, you’re reimbursed more, and the hospital gets more, as opposed to giving birth at home. And the fact is, is that about 85% of birthing people, for their first-time deliveries, they actually qualify for at-home births. But because we’ve had midwives erased, the role of them erased, their numbers have decreased substantially over the last century. And because the birthing process has been so medicalized, we’re seeing more people give birth in the hospital.
It actually also leads to more complications. So, if you give birth in a hospital, you’re more likely to have to have a C-section. You’re more likely to have to have other interventions, which actually leads to increased risk of death. And we also know that for Black birthing people, there is a higher rate of C-section for them, as well, which, again, you know, ties into health professionals and bias and why are they choosing to perform C-sections more on Black birthing people than other people.
So, all that to say is that our current system, where we have so many under- and uninsured people, where the birthing process has been medicalized, where midwife care has been erased — and we know that from other reports, like from the Commonwealth Fund, that actually having midwives involved in and other birth workers involved in the birthing process actually improves health outcomes. All of that has led to, you know, the poor maternal mortality rates that we see today.
AMY GOODMAN: My dad was an ophthalmologist, and he began his career at the National Institutes of Health. He looked at glaucoma, but he also looked at the effect of sickle cell on the eye. And I’m wondering if you can talk about the historical labeling of sickle cell as a so-called Black disease, and the impact on the perception and the research funding that then goes into it. And then talk about the history of your field, of emergency medicine, and where racism plays into that.
DR. UCHÉ BLACKSTOCK: Yeah. So, you know, I think, yeah, sickle cell disease, it was really important for me to write about it in my book Legacy, because of what I had seen in practice. So, I have seen the patients — especially at Kings County/SUNY Downstate in Brooklyn, I have seen so many of my patients coming into the emergency department with sickle cell disease and pain crises or other complications. And I began asking, you know, “Why do I keep seeing patients with sickle cell disease?”
So, what’s important for people to understand is sickle cell disease is an inherited disease. It is associated with a gene. And it actually does not just afflict people from sub-Saharan Africa. It afflicts people from the Mediterranean, from the subcontinent of India. So it’s not necessarily a Black disease. But because the majority of the people in the United States with sickle cell disease are Black, about 100,000 people, are Black, it’s been racialized as a Black disease in this country. As a result, there has been —
AMY GOODMAN: And explain what it is, just for people to understand —
DR. UCHÉ BLACKSTOCK: Oh, I’m sorry. Yeah.
AMY GOODMAN: — the sickling of cells and why it causes —
DR. UCHÉ BLACKSTOCK: Yes.
AMY GOODMAN: — such pain and it’s so dangerous.
DR. UCHÉ BLACKSTOCK: Sure. So, people with sickle cell disease, unfortunately, what happens is their red blood cells get misshapen. Because of the misshapen — or, they form like a sickle shape. And those cells, unfortunately, are not able to carry oxygen as well as normal red blood cells. And because they’re not able to carry oxygen as well, you know, oxygen delivery to different parts of the body is impaired and impacted. And so, as a result, when a person with sickle cell disease has a pain crisis and the cells are sickle-shaped, oxygen is not delivered to, you know, their heart, to their lungs, to their brain. And so people could come in with pain crises. So they have pain throughout their body. They can come in with lung infections. They can actually have strokes, as well. They can develop bacterial infections. It affects their spleen. So it’s actually a disease that can have very, very serious complications. Most people with sickle cell disease only live until their early forties.
But again, that is a result of the fact that this disease has been racialized as Black in this country. There has been a lack of funding towards research and innovation and developing therapeutics for sickle cell disease. There are about — are only about two therapeutics available for sickle cell disease, whereas other inherited diseases, like hemophilia, which is a bleeding disorder, and cystic fibrosis, which affects the lungs, they actually have multiple, multiple therapeutics to treat those inherited diseases, which actually afflict mostly white people.
And so, as a result of the lack of funding for sickle cell disease and the fact that there are very few sickle cell centers or a system that’s in place to really support patients with sickle cell disease, we end up seeing them very often in the emergency department. And because they often come to the emergency department in pain, they have been stigmatized as drug seekers, as people who are just there to get pain medication. And it’s been done in a really dehumanizing way. And I talk about how in my residency program, you know, my supervising residents and attending physicians would question me and say, “Well, are you sure that patient really has sickle cell disease? You know, send the test to make sure they do, or, you know, just give them only two pain medications and let them go.” And there was a lot of suspicion, a lot of doubt, when it came to caring for these patients with sickle cell disease. But I talk about how their treatment really is a result of the fact that this disease has not been funded properly. So they actually have to utilize the emergency department very, very often, because there is a system that is not in place to appropriately care for them.
AMY GOODMAN: And, Dr. Blackstock, one of the issues you take on in your book, Legacy, is, you know, walking out to treat a patient, and they say to you, “Oh, will you introduce us to the doctor, please?” Talk about what it’s meant for you to be a Black woman doctor in what is, surprisingly, still a white and often male world, though more and more women are involved.
DR. UCHÉ BLACKSTOCK: Right, yes. You know, I mean, as I said, growing up, I thought that most physicians were Black women, because that’s who I was surrounded by. My pediatrician was a Black woman, my mom. I went to conferences and meetings full of Black physicians and Black women physicians. So it wasn’t until I got older that I realized that that was a rarity and that wasn’t the case.
And, you know, when I talk about these experiences that — you know, for example, where a medical student, a resident, goes into a room, and then I come in, and they say, “I want to talk to that other doctor,” you know, it just is incredibly demoralizing and humiliating, too. Often, you just want to take care of your patients. But, you know, I’ve never been asked so much, you know, “Where did you go to school?” like, people really wanting to know and make sure that you actually are qualified to care for your patients.
So, I thought it was important in the book to talk about these experiences that not only I had as a patient, but also that I had as a Black health professional, because often these environments are inhospitable to us. And even, you know, microaggressions from our colleagues, microaggressions from our patients really can lead to attrition, can lead to really dissatisfaction with the kind of work we do. And so, that is why, with my organization, Advancing Health Equity, I really want to focus on making these environments where Black health professionals also can thrive and not just survive.
AMY GOODMAN: I want to thank you so much for being with us and give you a chance for your final message as you finish your book. I mean, this is a book about your life, your family’s life, about this country. But what most surprised you in doing the research for it?
DR. UCHÉ BLACKSTOCK: You know, I think what most surprised me is that the history runs so deep, that there are so many different examples, I couldn’t even — you know, I didn’t even have an opportunity to include in the book, of the history in this country that is actually so incredibly horrific, that explains why we are in the situations that we are today, why we see these profoundly horrific statistics. And I wanted to take that opportunity for this book to help even a broad audience, not just people in medicine, not just people in healthcare, to understand why we are where we are today, and what we can do about it. The last chapter, it’s a call to action for different groups. So I hope people will read that, feel galvanized and electrified to make a difference.
AMY GOODMAN: I thank you so much for being with us and, most importantly, for writing this book, Dr. Uché Blackstock, emergency medicine physician, CEO and founder of Advancing Health Equity, a company that works with healthcare organizations to fight racism and bias in services. Dr. Blackstock’s new book is called Legacy: A Black Physician Reckons with Racism in Medicine. Dr. Blackstock, her twin sister Oni and their mother Dale all graduated from Harvard Medical School, making them the school’s first Black mother-daughter legacies.
To see Part 1 of our discussion, you can go to democracynow.org. I’m Amy Goodman, with Nermeen Shaikh. Thanks so much for joining us.










Media Options