
Guests
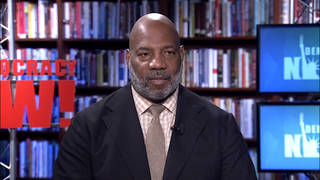
- Dr. Manuel Martinmedical innovation and access policy adviser for the Médecins Sans Frontières Access Campaign.
In response to the Food and Drug Administration’s full authorization of the Pfizer-BioNTech COVID-19 vaccine for U.S. residents aged 16 and over, Doctors Without Borders is calling on Pfizer-BioNTech to immediately share the vaccine technology with manufacturers on the African continent, where less than 2% of the population is fully vaccinated. Dr. Manuel Martin, a policy adviser at Doctors Without Borders, says it’s “regrettable but understandable” for rich countries to limit how many doses they export abroad, but “it’s completely unacceptable for countries to refuse to share the technology.” He also says rich countries should hold off on offering third booster shots to their populations while so many around the world are still waiting for their initial doses. “In the face of scientific uncertainty and given the historical vaccine inequity, I think really what should be prioritized is getting vaccinations to low- and middle-income countries and sharing the vaccine technologies.”
Transcript
AMY GOODMAN: This is Democracy Now!, democracynow.org. I’m Amy Goodman.
The Food and Drug Administration has fully authorized the Pfizer-BioNTech COVID-19 vaccine for U.S. residents aged 16 and over, making it the first COVID vaccine to be fully approved by the FDA. In response, Doctors Without Borders called on Pfizer and BioNTech to immediately share the vaccine technology with manufacturers in Africa, where less than 2% of the population is fully vaccinated. The medical humanitarian group is also urging the United States to demand the companies share information about the vaccines, which were created with significant public funding.
Pfizer has said it expects global sales of the vaccine to reach $26 billion this year. One study estimates it would take just $127 million for an existing manufacturing site to set up production and make 100 million doses. Doctors Without Borders say there are sites in Africa, including in Egypt, Morocco, South Africa, Tunisia, that could make 100 million doses annually within a 10-month time frame, but only if Pfizer shares the technology.
We’re joined right now by Dr. Manuel Martin. He is the medical innovation and access policy adviser for Doctors Without Borders’ Access Campaign, with Médecins Sans Frontières.
Dr. Martin, thanks so much for joining us. So, talk about what this full approval by the FDA means when it comes to global access to the vaccine.
DR. MANUEL MARTIN: Well, for now, the full approval just means the FDA considers this a safe and effective vaccine. Unfortunately, this doesn’t have direct consequences for global access. Perhaps even to the contrary, it might mean that supplies will be further restricted and we’ll see the continuing gap between vaccinations in high- and upper-middle-income countries versus lower-middle-income countries and low-income countries. And just to make that a little bit clearer, so far less than 1% of the doses have been delivered to low- or middle-income countries, whilst 99% of all doses have been delivered to countries that represent just 50% of the world’s population.
AMY GOODMAN: Even if the U.S. is only thinking of its own self-interest, you know, making sure the population is vaccinated, talk about what it means to have the world vaccinated for national security, in the United States or any country.
DR. MANUEL MARTIN: Well, whilst it’s understandable for countries — it’s regrettable but understandable for countries to try and limit the number of vaccines that are exported from the country, it’s completely unacceptable for countries to refuse to share the technology. It’s akin to sharing the recipe with other manufacturers, that would actually be multiplicative and wouldn’t take away any doses from the U.S. or any other high-income country.
AMY GOODMAN: I mean, looking at your press release, Médecins Sans Frontières, Doctors Without Borders, you say, “In an analysis by Imperial College of London commissioned by MSF, the estimated total cost needed for starting up mRNA vaccine manufacturing … and producing 100 million doses” — and we said this earlier — “is … $127 million for Pfizer-BioNTech’s vaccine and $270 million for Moderna’s vaccine. Considering the estimated $2.5 billion of public money that has gone into the development of mRNA vaccines — and the forecasted” revenue of, as we said, “$26 billion and $19 billion for Pfizer-BioNTech and Moderna, respectively — these companies have a public obligation to facilitate increasing vaccine production and supply wherever possible.” So, many people say, “Wait a second. While Moderna took money upfront from the U.S., Pfizer didn’t, but Pfizer got a guarantee of sales in the U.S.” Talk about this public money and what exactly it would mean for companies around the world, factories that didn’t invent the mRNA vaccine but do have the ability to scale up and make it.
DR. MANUEL MARTIN: Well, we have to think of public funding, indeed. You mentioned the advance purchase agreements, which, if they were made very early, are a way to derisk research and development expenditure. But we also saw the partner company, BioNTech, receive quite a substantial amount — in fact, 450 million U.S. dollars from the German government. So it’s not only the U.S. that has been funding the research and development of these companies. And like you point out, the profits that these companies are likely to make, independent of whether the technology is shared or not, is in the tens of billions this year. And there’s really no reasons why they shouldn’t share that with other manufacturers. If they would, we would likely see a multiplicative effect, where we would have many manufacturers in low- and middle-income countries producing the vaccine. And a decentralized manufacturing model would really also reduce the risk of very narrow political export controls, for instance, limiting vaccine supply, like we have seen, for instance, with the U.S., but also with India.
AMY GOODMAN: The World Health Organization is calling on wealthy countries to impose a booster moratorium on COVID shots. Let me play a clip.
TEDROS ADHANOM GHEBREYESUS: At present, just 10 countries have administered 75% of all vaccine supply, and low-income countries have vaccinated barely 2% of their people. I called for a temporary moratorium on boosters to help shift supply to those countries that have not even been able to vaccinate their health workers and at-risk communities and are now experiencing major spikes. Last week, WHO brought together 2,000 experts from all around the world and debated the available data on boosters. What is clear is that it’s critical to get first shots into arms and protect the most vulnerable before boosters are rolled out.
AMY GOODMAN: So, that is WHO [director]-general. Your response, Dr. Martin?
DR. MANUEL MARTIN: Well, and what we are weighing up right now — and I think Dr. Tedros is completely correct — is the possibility of boosters saving some lives in high-income countries versus the certainty of first vaccinations saving many lives in low- and middle-income countries. That is the option. And I think in the face of scientific uncertainty and given the historical vaccine inequity, I think really what should be prioritized is getting vaccinations to low- and middle-income countries and sharing the vaccine technologies.
AMY GOODMAN: And what would you say to companies saying, “Then we can’t guarantee the quality, if we give over the recipe and the technology to these companies and factories that we’re not familiar with”?
DR. MANUEL MARTIN: Well, I would say that is an incredibly paternalistic view of manufacturers in low- and middle-income countries. There are many manufacturers in low- and middle-income countries that are very capable of producing high-quality vaccines, that are approved, actually, by regulators in Europe and even by the FDA. So that’s really not a good excuse for not sharing the technology.
AMY GOODMAN: Dr. Manuel Martin, I want to thank you so much for being with us, medical innovation and access policy adviser for Doctors Without Borders, Médecins Sans Frontières, MSF. He was speaking to us from Portugal.
Coming up, Governor Cuomo commutes the sentence of former Weather Underground member David Gilbert. It was one of Cuomo’s last acts before he resigned at midnight last night. We’ll speak with David Gilbert’s lawyer. Stay with us.










Media Options