
Topics
Guests
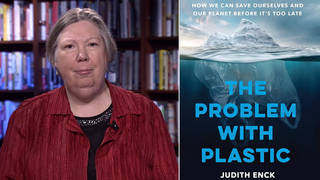
- Sheri Finkreporter for ProPublica and an MD. She’s worked with humanitarian aid organizations here in the United States and overseas, and she’s the author of the acclaimed 2003 book War Hospital: A True Story of Surgery and Survival. Her latest article, jointly published on ProPublica.org and the New York Times is titled “The Deadly Choices at Memorial.”
On the fourth anniversary of Hurricane Katrina, a major investigation reveals harrowing new details of one of the many human tragedies that occurred in the aftermath of the storm. Forty-five patients at the New Orleans Memorial Medical Center died in the days after Katrina’s floodwater knocked out the power in the hospital. A 13,000-word article titled “The Deadly Choices at Memorial” tells the full story of what really happened to some of those patients. It’s the cover story of the New York Times Sunday Magazine this weekend and the product of a two-and-a-half-year investigation. We speak with reporter Sheri Fink of ProPublica. [includes rush transcript]
Transcript
ANJALI KAMAT: It’s four years after Hurricane Katrina devastated New Orleans. As the floodwaters rose, we read a text message from New Orleans attorney Bill Quigley from inside Memorial Medical Center, where he went to stay with his wife, a nurse at the hospital. The text message from August 31st, 2005, said, quote, “no water, sick, no heat, call somebody for help.”
This is how he described the scene when we reached him over the telephone the next morning.
BILL QUIGLEY: At this point now, there’s about five-plus feet of water outside the hospital, and they’ve lost power in the main stairwells. The power is reduced throughout the entire building. We don’t have air conditioning, and the building is sealed, so you can’t open to get, you know, even a breeze, so it’s pretty hot in here. And on the upper floors, they don’t have enough water pressure to be able to use the toilets and that. So we have areas that don’t have electricity, areas that don’t have any water pressure. And the water is rising, and shortly, when the water gets high enough, we will lose the electricity that we do have and the internal communication abilities that we have.
ANJALI KAMAT: New Orleans attorney Bill Quigley. We reached him on the telephone September 1st of 2005, speaking from inside Memorial Medical Center.
That was only the beginning of the horror. Today, we go to a major investigation that reveals harrowing new details of one of the many human tragedies that occurred in the aftermath of the storm. Forty-five patients at the Memorial Medical Center died in the days after Katrina’s floodwater knocked out the power in the hospital.
A 13,000-word article titled “The Deadly Choices at Memorial” tells the full story of what really happened to some of those patients. It’s the cover story of the New York Times Sunday Magazine this weekend and the product of a two-and-a-half-year investigation by ProPublica reporter Sheri Fink.
The piece investigates allegations that some of the medical staff at the hospital euthanized those patients who were deemed to be the sickest and had signed Do Not Resuscitate orders. It reveals more patients than were previously known had been injected with drugs intended, as one doctor put it, to hasten their demise. Not all of the patients were on their deathbeds at the time of the injections.
AMY GOODMAN: Dr. Ewing Cook, who had not been previously interviewed, told Sheri Fink he gave a seventy-nine-year-old woman with uterine cancer and kidney failure medicine to, quote, “get rid of her faster, get the nurses off the floor.”
Louisiana’s Attorney General Buddy Caldwell told the Associated Press Friday he would not reopen a probe into the deaths. His predecessor Charles Foti had arrested Dr. Anna Pou and two nurses in July of 2006 in connection with the deaths of four patients. A grand jury declined to indict them in 2007.
Well, for more on this story, we’re joined here in our firehouse studio by the author of this haunting, explosive investigation, Sheri Fink. She’s a reporter for ProPublica and an MD. She’s worked with humanitarian aid organizations here in the United States and overseas. She’s the author of the acclaimed 2003 book War Hospital: A True Story of Surgery and Survival.
Sheri Fink, welcome to Democracy Now!
SHERI FINK: Thank you.
AMY GOODMAN: Talk about this journey you have taken over the last two-and-a-half years, the first — the first hint you got of what’s going on and how you pursued this investigation.
SHERI FINK: Well, I think I heard about it just like most people, with the arrest of these well-respected health professionals in New Orleans on charges of second-degree murder. And I had worked in disaster situations myself, delivering humanitarian aid, and so the issue really just caught my attention, and I wanted to know more.
AMY GOODMAN: So, lay out for us, as you understand it, day by day, what happened at Memorial Hospital as the hurricane hit and then the waters rose.
SHERI FINK: Well, the hurricane hit in the very early morning hours of Monday, August 29th, 2005. And the hospital did pretty well. It sustained quite a lot of damage in terms of, you know, the money that it would have cost to fix it, many windows broken and water damage, but, in general, it was a functioning place. There was backup power. There were still communications. And everything seemed OK. People breathed a sigh of relief.
Well, the next morning, that’s when they saw the water starting to rise around the hospital, on Tuesday. And as your — as Bill Quigley said in that phone call, they knew that if the water got to a certain level, that would just knock out the power, knock out the backup power, and so they immediately started evacuating. And, of course, they did what many of us would think was very logical: get the people out who rely on machines, who — even at this point, on the backup power, like in many hospitals, backup power does not power your air conditioning. Well, imagine a ninety-some-degree day in New Orleans, sealed hospital, temperatures going up into, you know, above a hundred. So, very quickly, they started to evacuate the patients in the ICUs, the pregnant mothers, the little NICU babies, babies in the neonatal ICU.
Well, that night, the power went out, and a group of patients who had not been evacuated — there was a decision not to evacuate anybody with a DNR order, “do not resuscitate.”
ANJALI KAMAT: Who made this decision?
SHERI FINK: This decision was made by the doctors, when they were trying to prioritize who should get the first slots on the evacuation helicopters. And it was sort of — it was described to me in different ways. But nobody really disagreed with it. One doctor said people with DNRs generally have terminal or irreversible conditions. You know, this is how he rationalized it. And therefore they would have the least to lose in case there was some calamity. Another doctor said, “Well, these people have signed up. They said they don’t want any kind of extraordinary means to keep their lives going. And so, we’ll just translate that into this disaster and believe that they wouldn’t want the first slots on the evacuation helicopter.”
Well, it turned out that that wasn’t so simple. People with DNR orders have them for lots of reasons. DNR just means, don’t restart my heart if it stops, don’t restart my breathing, don’t give me CPR. It doesn’t necessarily mean that somebody is on their deathbed. And indeed, many family members in the hospital really disagreed with this decision when they found out about it. They weren’t part of that decision making, which is one of the, I think, the big lessons of this story, is that, in the future, when we think of swine flu or other kinds of health issues where there are limited resources, that really people need to be part of that conversation, need to be weighing in on what we want our priorities to be. And indeed, numerous family members at the hospital requested that the DNR orders be taken off their loved ones.
AMY GOODMAN: Tell us one of those stories.
SHERI FINK: Well, one story would be Angela McManus, who was the daughter, a very devoted daughter, of a colon cancer patient up on the LifeCare floor. Now, this was the other group of people who didn’t get evacuated first. There were about fifty-some long-term acute care patients in a hospital within a hospital on the seventh floor of Memorial. And long-term acute care means people who have multiple medical problems, often elderly, some near the ends of life, but people who need to stay in a hospital for a long time and often need ventilators, need to rely on machines. For some reason, these people weren’t thought of in that initial meeting, and so they stayed. And when the power went out, their conditions really declined very quickly.
And so, then we go, a day later, helicopters stop coming. It’s Wednesday, hot in the hospital. All the patients have been moved down to the main floors to kind of stage them for a quick evacuation, thinking that the helicopters would keep coming. And suddenly, that all slows down. Get some people out by boats, but they have to go and wade through water to get to dry ground after the boat drops them off. They don’t even know if there will be ambulances there, so mainly healthy people would go out that way. And suddenly, the staff decided, let’s get the healthy people out first, and let’s prioritize all of the sickest patients last. This was a decision that they made in their triage.
And so, the people who were the very sickest started to really languish, and that’s when these discussions about “Should we consider euthanasia? Should we consider hastening people’s deaths? Are they suffering too much? What should we do about this?” — that’s when those conversations started.
AMY GOODMAN: Or “Are they simply too fat to bring downstairs?”
SHERI FINK: Well, this was another very — probably one of the most disturbing incidents that I described.
AMY GOODMAN: Sheri, we’re going to get to that after break. Our guest is Sheri Fink, who has done an explosive exposé that she has worked on for more than two-and-a-half years, reporting for ProPublica and together with the New York Times Magazine. It was just published on Sunday. This is Democracy Now!. We’ll be back with Sheri Fink in a minute.
[break]
AMY GOODMAN: Our guest is Sheri Fink, reporter for ProPublica, and she’s also a doctor. And she works with — had this piece published in the New York Times Magazine, a remarkable piece that took up more pages than I’ve almost ever seen in the New York Times Magazine, a piece that on the cover said, “The floodwaters from Katrina had knocked out the power. Doctors and nurses were overstretched and overtired, patients were dying and the evacuation of many of the sickest seemed impossible.
“Injecting drugs was one answer that some members of the medical staff decided on. Were they trying to comfort those patients — or hasten their [demise]?”
Anjali?
ANJALI KAMAT: Sheri Fink, in your article, you describe very movingly the way the system of triage worked itself out at Memorial Medical Center. You talk about patients being labeled “1’s” and “2’s” and “3’s.” Can you explain this?
SHERI FINK: Sure. Well, this was just horrifying for anybody who walked by or any of the staff who had to participate in it, but basically they decided to triage, which means sort. It’s a word that goes back to the time of Napoleon and trying to figure out how to prioritize who gets treated first on a battlefield when there are lots and lots of injured people and not so many medics to take care of them. So, in a similar way, the doctors in this hospital, like most doctors in America, had very little experience with anything like wartime triage.
And there are many different systems by which you can do triage, and they haven’t really — particularly when you think about a hospital population with a lot of chronically ill people, not a war zone, not acutely injured people, there isn’t so much evidence on how you decide who has the best prognosis, who has the worst prognosis. But this staff attempted to do this.
The “1’s” were the people who were ambulatory, the walkie-talkies, the people who could get out by boat and walk. The “2’s” were slightly more sick, might need some help, might be in wheelchairs, need some help getting out. And the “3’s” were this group of the sickest patients, patients who were bed-bound and who would need to go out by helicopter. And as I mentioned, on Wednesday, August 31st, the decision was made that the 3’s would go last.
ANJALI KAMAT: And can you talk about the case of Emmett Everett? You were just starting to tell us that story before we went to break, the Honduran worker who was up on the seventh floor.
SHERI FINK: That’s right. So, he had received a three. But Mr. Everett was not ambulatory, because he had had a spinal cord stroke, which is a very rare thing which left him paraplegic. And he had multiple medical problems, as most people in a long-term acute care facility did. He was waiting for a surgery to help ease a chronic bowel obstruction.
But he was very much aware of what was going on. The helicopters, you could —- actually, the seventh floor of LifeCare looked out onto the helipad, and you could even feel the propeller wash, people told me, when the helicopters would land. His roommates were taken down, and he was still left in his room. And he asked people, the nurses; he said, “Don’t let them leave me behind.” He had -—
AMY GOODMAN: He was fully coherent and cognizant of everything happening.
SHERI FINK: Coherent, fed himself breakfast that morning, said, “Are we ready to rock and roll today?” He was a very — people describe him as a really, really wonderful man, great sense of humor, didn’t dwell on, you know, his problems.
And so, according to witnesses and Dr. Anna Pou, the one — the doctor who had been arrested — she has chosen not to speak about what she did on Thursday, September 1st, ’05, citing some ongoing legal wrongful death lawsuits by patients’ families, including Mr. Everett. Witnesses, other staff on the LifeCare floor say that Dr. Pou arrived, came up to the floor that morning, said, “I don’t think” — you know, said that the patients are not going to get out. And other staff on the floor thought that most of them looked bad and said, “Sure,” that that — “You might be right.” And she said, “I think that they’re not aware. Most of them aren’t conscious.” And they said, “Well, actually, that’s not true. We have Emmett Everett here, who’s very conscious and very aware.” And —-
AMY GOODMAN: Who, as he said, was ready to rock and roll.
SHERI FINK: Ready to rock and roll, wanted to get out. And apparently, according to several people who later spoke with investigators, a discussion was had in which they talked about how they might get him out, and they decided that because he was so heavy and it was so hot and people had -— I mean, just imagine. It’s hard for us. We’re sitting here, and it’s air-conditioned. They had been going on no sleep for days, the medical workers. They were tired. They were terribly disturbed by all the suffering that they felt that they saw around them. And so, in this sort of moment, they apparently decided that he could not be brought down, could not be evacuated, that there was no way to get him out.
I did speak with people who were working on transporting patients and up on the helipad, getting people out, and they said, “Are you kidding? Of course, if we had known about him, we would have made that effort. We could have gotten him out. We got out someone who was 500 pounds on a mattress on the bottom of a boat, who was an amputee.” So there were examples of people this size who did get out.
AMY GOODMAN: Even in the hospital?
SHERI FINK: In this hospital.
AMY GOODMAN: Even in the hospital, there was someone who was more than 300 pounds —-
SHERI FINK: Yes.
AMY GOODMAN: —- that they wheeled into the helipad, and they were able to get him out?
SHERI FINK: Yeah, there was one who’s described in the article who got out by helicopter, and he was the last patient out. Mr. Scott, his name was. And there was at least one patient who was well over the weight of these patients who went out by boat. So it’s hard to know exactly why this decision was made or what exactly happened.
All we know is that Dr. Pou was seen going into this patient’s room with medications, saying, “I’m going to tell him I’m going to give him something for his dizziness.” And later, during the investigation, he had died, and they found these drugs, morphine and midazolam. These two drugs that were found in many of the patients were found in him. So it’s hard to know exactly what happened there.
AMY GOODMAN: Can you, Sheri Fink, tell us a little more about Dr. Anna Pou, what she was doing at the hospital, the indictment – rather, the grand jury, the decision not to indict, and what she’s doing now?
SHERI FINK: Sure. Well, Dr. Pou is an extremely well-respected head and neck surgeon, from everything I’ve been able to gather, just very, very dedicated to her career and her patients, just sacrifices a lot to give them her cell phone number. Patients of hers I spoke with just raved about her. This is the kind of doctor that everybody would want, just totally dedicated doctor, very compassionate doctor.
And she was, you know, seen by many people injecting these medicines, you know, allegedly saying that she was giving lethal doses, something that she very much denies that she said. She talks, in fact, about — she was giving medicine to people for pain and for comfort. So that’s how she’s described this. And a grand jury agreed with that, apparently. They were asked to look at whether she should be indicted for second-degree murder, and they decided not to. And part of this story goes into the very difficult kind of dilemma that the coroner faced trying to decide whether these were homicides or not.
ANJALI KAMAT: Sheri Fink, I want to turn to a September 2006 interview with Dr. Anna Pou from CBS’s 60 Minutes. The Louisiana State Attorney General Charles Foti had recently said the deaths at the nursing home were not a result of euthanasia, but, quote, “plain and simple homicide.” Dr. Pou spoke to Morley Safer of CBS News.
DR. ANNA POU: It is unbelievably shocking for me that I’m actually sitting here having this conversation with you on national TV. And I want everybody to know that I am not a murderer, that we are not murderers.
MORLEY SAFER: What was the evacuation plan that you had?
DR. ANNA POU: The evacuation plan that we had was to get every single patient out of that hospital as quickly as we could.
MORLEY SAFER: Were people dying?
DR. ANNA POU: Yes, people were dying.
MORLEY SAFER: From their diseases or from the conditions?
DR. ANNA POU: You have to understand that there were very sick people in the hospital, because if they were not sick, they wouldn’t have been there. You have this intense heat. You have — you know, we have the lack of all the tools that we normally use. You know, we have monitors and ventilators and all the tools of modern medicine; we didn’t have those to use anymore. We didn’t have any of those. And so, a lot of these patients could not tolerate the conditions and the severe heat and the dehydration, and a lot of people succumbed to that. People were dying from the horrible conditions, because they were not strong enough to tolerate them.
MORLEY SAFER: I know you don’t want to go into specifics about treatment on Thursday. But just in general, how do you feel about the way you handled the situation, in terms of your treatment of the patients?
DR. ANNA POU: I don’t think that I could have done anything more. I worked almost around the clock running up and down the stairs. I did whatever was humanly possible that I could possibly do to take care of these patients, and not only the patients, but their family members, the nurses, their family members. I mean, we were all working as a team, and we were all taking care of each other.
AMY GOODMAN: That was Dr. Anna Pou in 2006 on 60 Minutes. Sheri Fink, she did not talk to you?
SHERI FINK: She did speak with me. She was very generous with speaking with me, gave me a bunch of time last year. But she was not — when I walked in for the interview, the lawyer said, “Just don’t ask her any questions about Thursday, September 1st,” the day where she was alleged to have done these things. And he explained that, being that she still had these wrongful death lawsuits. So we spoke extensively about Monday, Tuesday, Wednesday, and, as she said, just the hard, hard work that she and others put in. I mean, she really was — people —- kind of at the center of things and working so very hard.
AMY GOODMAN: So, explain. How many people died? How many people had these chemicals in their body? Talk about the chapel, which became the mortuary.
SHERI FINK: That’s right. So, what my investigation found was that at least a dozen and a half patients were found after their deaths to have morphine, midazolam and/or both. And I should say -—
AMY GOODMAN: You mean eighteen people?
SHERI FINK: Yes, at least eighteen people who had — seventeen of them received those injections shortly before their deaths on Thursday, September 1st, so after a sort of, you know, major evacuation of the hospital had begun.
Helicopters had belatedly and finally converged on the hospital that morning. Everybody was being told, “You got to get out. You got to get out.” There were a lot of fears of the neighborhood, fears of gunshots, police on the emergency room ramp saying, “You got to get this hospital cleared out by 5:00, or else, because we’re leaving, because it’s too dangerous at night.” So, I just want to give you guys a sense of the feeling in that hospital at the moment that these drugs were injected.
And the new — I guess the news in my article, number one, is the number of patients that received these drugs, because Dr. Pou had been arrested in the cases of four patients, that there were at least a dozen and a half. And number two is that some professionals, doctors and nurses, were willing to talk about why they gave these drugs. So, Dr. Pou didn’t, but two doctors and a nurse did. And they describe a variety of reasons for why they still, to this day, feel that that was the right thing to do for these patients.
AMY GOODMAN: I mean, the description, for example, of the LeBlancs, the husband and wife who got a flotilla of boats to come get Mr. LeBlanc’s mother, who was in LifeCare —-
SHERI FINK: Right.
AMY GOODMAN: —- who was on the seventh floor.
SHERI FINK: Mm-hmm.
AMY GOODMAN: Very quickly, what happened?
SHERI FINK: Sure. Well, this was a couple — many people that had their family members in the hospital felt it was the safest place for them to be. This hospital had been around since 1926, and no problems. They had left their mother there, who had many medical problems, and had evacuated for the hurricane, as told, that the city was a mandatory evacuation, except for the hospitals. And when they heard what was happening, they just shot back into the city. They talked their way in. Sandra, the wife, was an EMT. They managed to find some other would-be rescuers and direct boats to the hospital to help evacuate it on Wednesday. And these were airboats, the sort of fishing boats that you find a lot in Louisiana. And they managed to take lots and lots of people out, not just their mother, but they spent the whole day going back and forth evacuating people to dry ground.
AMY GOODMAN: They got their mother, but after they had to fight the authorities at the hospital saying they couldn’t take her.
SHERI FINK: Yeah, it’s not clear why. I mean, their mother was given a three. She was DNR, so she was prioritized to be last in the evacuation.
AMY GOODMAN: Do not resuscitate.
SHERI FINK: Yes.
AMY GOODMAN: Could have been injected.
SHERI FINK: Could possibly have been injected the next day. They don’t know. You know, nobody knows. But what they do know is that they went and tried to take her out. Maybe some doctors who didn’t know who they were said, “No, you can’t take this patient.” And they said, “The hell we can’t,” and they lifted her up and put her on the boat. And she was — apparently, she was chatting and smiling and sort of amused by the whole thing. She wasn’t disturbed by it.
AMY GOODMAN: And your response, finally, to the attorney general saying they will not reopen this investigation?
SHERI FINK: Well, I think, you know, again, the conditions. If you read the story, you’ll see just how extraordinary the conditions were. You know, many people said to me, “We just did the best we could.” And so, there’s the question of whether something fits the definition of a particular crime, whether an action fits that definition, and then whether you want to prosecute it. And those are two separate questions, and I’m not a lawyer. And I think that those are questions that perhaps, after we read this story, individuals can decide for themselves what they think about that.
But the larger point being that let’s not let this ever happen again. Let’s not ever have such a failure of government and of larger systems that doctors and nurses and patients are put into this situation. That’s my hope.
AMY GOODMAN: Well, Sheri Fink, thank you very much for joining us and for spending two-and-a-half years investigating this story, a remarkable piece of investigative journalism. Sheri Fink, a reporter for ProPublica, she’s a doctor, and she had her piece published in the New York Times Magazine on Sunday.











Media Options