
More than 40 countries have temporarily suspended some or all travel from the United Kingdom after British health officials announced a highly infectious variant of the novel coronavirus has been spreading in the country. South Africa has detected a similar variant. The new variant is believed to be 70% more contagious, but health experts say existing vaccines will still be effective against it. “What’s important to remember is that mutations will naturally happen in the course of a virus that’s in the community and circulating,” says Dr. Taison Bell, critical care and infectious disease physician at the University of Virginia. “It’s not unexpected to have these changes.” Bell also describes how he received the Pfizer-BioNTech COVID-19 vaccine earlier this month.
Transcript
AMY GOODMAN: This is Democracy Now! I’m Amy Goodman, with Juan González.
The number of nations banning travel from the United Kingdom continues to grow in response to the new, highly infectious variant of the coronavirus British health officials announced over the weekend, throwing much of Britain into strict lockdown. South Africa has detected a similar variant. More than 40 countries have temporarily suspended some or all travel from the U.K., including Canada, Chile, France, Ireland and Hong Kong. The United States has not announced a travel ban with either England or South Africa. On Monday, Washington state Governor Jay Inslee announced his state would require those arriving from either country to quarantine for 14 days upon arrival.
British officials claim the new variant could be 70% more contagious but is not thought to be more deadly. Many scientists are skeptical of the claim, which has not been peer-reviewed. Experts also say it’s possible the coronavirus variant didn’t develop in the United Kingdom but instead was detected there first because of Britain’s extensive monitoring system and giving it to an international database, thousands of the code, so that other countries — of the genetic sequence — could analyze what they have. The United States doesn’t share that kind of information as widely.
On Tuesday, BioNTech CEO Ugur Sahin said he was confident the COVID-19 vaccine would work on the new variant.
UGUR SAHIN: We are going to evaluate that in a test, so we will build this new mutation into our assay system, and we’ll evaluate if the immune response against our vaccine is able to inactivate also this virus variant. We are confident that this will be the case, since in the past we have tested more than 20 virus variants with different type of mutations, and the result was always that the vaccine induces immune response which is so broad and that it attacks multiple, multiple positions in this virus protein.
AMY GOODMAN: This comes as the United States recorded more than 200,000 new coronavirus cases Monday, nearly 2,000 COVID-19 deaths. U.S. hospitalizations hit another world record high, topping 115,000, and 16 states recorded a record number of new deaths.
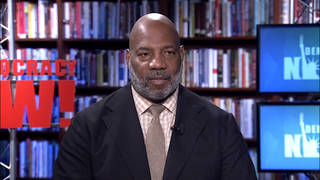
For more, we’re joined in Charlottesville, Virginia, by Dr. Taison Bell, a critical care and infectious disease physician at the University of Virginia who received the Pfizer-BioNTech COVID-19 vaccine earlier this month.
Dr. Bell, welcome to Democracy Now! We’re talking global, but let’s go right to the molecular and just personal level. How did it feel to get this vaccine? What should people expect? And why did you decide to be among the first to get this? Dr. Bell, can you hear me?
DR. TAISON BELL: I can hear you.
AMY GOODMAN: Oh, can you talk about your own experience in getting the vaccine, and how it felt?
DR. TAISON BELL: Oh, sure. I received the vaccine last Tuesday and just had a little bit of injection site pain initially, but then, right after that, a little bit of arm soreness, which has been commonly reported. But the day following, I felt completely fine and have no symptoms whatsoever. Important to point out that a lot of people who did have some of the other symptoms, like maybe low-grade temperature or fever or chills, it was after the second dose. So, after that second dose, we’ll see. But so far, so good.
JUAN GONZÁLEZ: Could you address some of the issues that have been raised about reported side effects? Should people be concerned about issues like Bell’s palsy or allergies? Is it severe allergies, or is it allergies in reaction to a previous vaccination?
DR. TAISON BELL: Yeah, that’s a good question. Now, to address the issue of Bell’s palsy, there was a numerical difference in the number of patients who had Bell’s palsy in the clinical trial — I believe it was four — in the Pfizer trial, in who got the vaccine, compared to zero, who did not. Now, what confuses that is that there’s a baseline rate of Bell’s palsy in the community just without a trial happening in the first place, and the numbers kind of match up with those numbers. So it’s hard to tell whether it was due to the vaccine itself or not. At this point, it doesn’t seem to be a signal there, but we’ll get more data as it goes on.
The issue with allergy is a little more nuanced. So, we have seen the reports of people in the U.K. and in Alaska who had these anaphylactic or anaphylactic-like reactions, which are severe reactions to the vaccine. Now, the recommendation is to only not receive the vaccine if you have a history of severe allergies to one of the known components of the vaccine itself. So, Pfizer lists their 10 components in the vaccine; Moderna has their list, as well. Most of these are things like salts, sugars and fats to keep the mRNA molecule stable. There’s a stabilizing molecule called polyethylene glycol that allergists think could be potentially responsible for these severe reactions. And for all intents and purposes, unless you have those reactions, the recommendation is to go ahead and get the vaccine, but if you do have a history of severe allergic reactions, to just wait a little bit longer than the usual 15 minutes and wait 30 minutes after the injection to make sure that you don’t have these allergic symptoms. In all these cases, the workers were in that monitoring period and were able to receive the treatment that they needed.
JUAN GONZÁLEZ: And could you talk about the rollout of the vaccine, and specifically the priorities recommended by the CDC in terms of who should get it? Because, obviously, especially after the — even within the first group of frontline healthcare providers, there’s a lot of leeway there. I mean, for instance, we’ve all seen how Sanjay Gupta of CNN, a surgeon and a journalist, got a shot in the first week, even though he does not directly deal with COVID patients, as being a surgeon. So, even within the medical community, there are people who are actually frontline and those who are in other fields or administrative. And then, when you get to the second priorities, the first responders and people over 75, among the first responders, there’s huge variety. You could be a police captain or a deputy inspector, who never comes in much contact with the public, versus a beat cop, who might regularly come in contact, not only with people he has to arrest, but homeless people and others. Could you talk about how you determine — how a locality determines which people within the priority group should get the vaccine first?
DR. TAISON BELL: Well, that is a difficult question, but I think what we should focus on is an equity distribution, so equitable lens and thinking about who are our highest-risk providers, initially, who are providing frontline COVID care, and then hospital workers in those communities that are also at high risk for encountering people with COVID-19.
Now, we have an example recently that Meharry Medical College and their affiliate hospital, Nashville General, were skipped over for the initial Pfizer vaccine shipments. Now, Meharry Medical College is the nation’s largest private, historically Black academic sciences center. They have been leading on the front for combating COVID-19, and their workers are extremely high-risk. Now, not only that, their president and CEO, Dr. James Hildreth, is on the advisory committee to the FDA that initially reviewed and approved the vaccine. There is no way that they should have been skipped over in initial shipment of vaccine. Turns out the state plan actually focused on larger institutions like Vanderbilt but left out smaller institutions like Meharry and saved them for the Moderna vaccine. And Dr. Hildreth actually had to get doses of the Pfizer vaccine from a separate hospital system.
Now, if we think about this through an equity lens, we need to think about places like Meharry initially and change the conversation from “Should we distribute early vaccine to places like this that are extremely high-risk, that serve a higher-risk community?” It’s not “Should we distribute,” but “We need to distribute to places like this, and how do we overcome the hurdles if there are logistical ones there?” So, if places like Meharry can struggle and be left out, then any facilities that serve Black and Brown communities is at risk. And that’s why we have to change our focus and think about equitable distribution.
AMY GOODMAN: If you can talk, Dr. Bell, about the reports of the mutation of this virus? It is not a different strain; it is a variant. It looks like Britain is being basically shut off from Europe right now, with this reported variant that could be up to 70% effective, or maybe it’s just so well documented because they’re sharing these gene sequences with the world through an international database, that the U.S. has not contributed to very much, so we don’t know as much about what’s happening in this country. But the significance of both Britain, also South Africa, and what this means, though the head of BioNTech says that they have taken into consideration these various variants, and it will be covered by the vaccine, for example, that you took, Dr. Bell?
DR. TAISON BELL: Exactly. So, the variant that’s been circulating is a relatively recent discovery but was thought to have occurred beginning in September in the southern part of the U.K. And now we have seen that it has become one of the more dominant species or dominant variants of the vaccine — or, the virus itself.
Now, what’s important to remember is that mutations will naturally happen in the course of a virus that’s in the community and circulating. And luckily for us, the coronavirus actually does not mutate at the same rate of viruses like influenza or HIV, which is a good thing. So it’s not expected to have these changes and variants in the community. Now, the researchers who came up with the vaccine knew this, of course, and planned for it.
So, the spike protein, for instance, which is the protein that is training our immune system to make antibodies against the coronavirus, it’s actually a complex, three-dimensional structure, and our immune system generates antibodies at different parts of it. So, for instance, if you were to go outside and see a baby, and then you come back later and see that the baby is asleep, you still recognize it as the same baby even if his eyes are closed or there’s a blanket over it. There are different ways for you to recognize what something is. And likewise, the immune system has to figure out if something is a friend or foe. So, even if one part of that mutation is a little bit different, you have other antibodies to recognize it, and you can still recognize whether something is a friend or foe.
Now, down the road, is there that possibility that there are so many changes that the protein might change enough that we might have to update that vaccine? You know, sure, that’s a possibility. We’re not sure if that’s going to be the case. But if that were to happen, the scientists are already on it, and they have a plan to update it if they need to.
So I think the main thing to think about with this variant is that it does appear to be more transmissible. And that means our public health practices are going to have to be even more important, like social distancing, wearing a mask, washing your hands, avoiding tight-packed indoor closed spaces. And then, the vaccine should still work at this point.
JUAN GONZÁLEZ: And, Dr. Bell, I’m wondering if you could talk about what the past nine months have been like for you. You’ve been overseeing the COVID-19 care unit at the University of Virginia. And personally and politically, what kind of toll has this taken on you, as you’ve been dealing with this day in and day out?
DR. TAISON BELL: I think, you know, I could join many healthcare workers in saying it’s been a personal hell. You know, there’s no other way to describe it. This is a disease that has ravaged the community and has affected every part of our lives. And no one person has been spared, whether it’s been you contracted COVID yourself, you’re taking care of COVID workers, you have family members or colleagues or friends who have contracted COVID-19, or you’re being affected by the shutdowns and the turndown in the economy or children not in school. We’re all dealing with this in some form or fashion. And it’s disproportionately affecting the Black and Brown communities, so people that I know and I love, and my own family members. It’s absolutely horrendous, what we’ve been dealing with.
And that’s why it was so important, that moment I received the vaccine, because I felt a little bit of a burden being lifted. Of course we have a long way to go. But there’s hope now. And we just have to get to the light at the end of the tunnel. And there are still some dark days ahead, but we can get there, but it’s going to take a big effort and continued vigilance on our part.
AMY GOODMAN: Finally, Dr. Bell, I couldn’t help but think, as we learned about the state of Virginia taking down the statue of the Confederate General Robert E. Lee from the U.S. Capitol, from Statuary Hall, and replacing it by a civil rights pioneer, Barbara Johns, who organized a student walkout to protest segregated schools in Virginia, who was involved in a lawsuit that became part of the landmark Brown v. Board of Education case — thinking about those kind of statues being tumbled and the kind of work that you’re doing. Your final message, not only to Black Charlottesville — you’ve been documenting your own journey along the way — but to people throughout this country and around the world, when it comes to dealing with COVID and who gets treated, who doesn’t?
DR. TAISON BELL: Well, I think that, you know, the symbolism that we put in our society matters. And, of course, their actions matter, as well. It’s not lost on me that I work at an institution that was founded by a member of society who was highly esteemed but thought that people like me were unworthy of being educated, had disagreeable body odors and were subhuman. And I walk into an ICU, and I take care of patients, and I’m trying to save lives for the Commonwealth of Virginia. So, that is not lost on me.
AMY GOODMAN: You’re talking about Thomas Jefferson?
DR. TAISON BELL: I definitely am talking about Thomas Jefferson. And, you know, what we have to remember is that we have to take down our symbols that are honoring legacies that do not agree with our true nature of American democracy, but we also have to take action and to make sure that our actions speak for our words. So that means focusing on equitable distribution, thinking about Black and Brown communities from the outset instead of making them an afterthought. And it means making sure that we get into these communities and break down the barriers that have historically existed between academia and institutions and the community itself. This is a chance where we can actually make true partnership with our communities that need us the most, and we have to take that chance and make that opportunity.
AMY GOODMAN: Well, we want to thank you so much, Dr. Taison Bell, critical care and infectious disease physician at University of Virginia, received the Pfizer-BioNTech COVID-19 vaccine earlier this month, joining us from Charlottesville.
Next, we look at how President Trump has raised over half a billion dollars since mid-October as he tries to overturn the election. How much of that money is going into his own pocket? Stay with us.










Media Options