
Topics
Guests
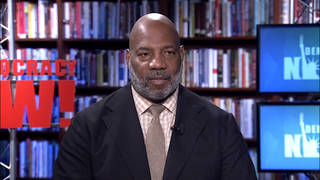
- Dr. Homer Ventersphysician and the former chief medical officer for New York City’s Correctional Health Services. He is currently the senior health and justice fellow at Community Oriented Correctional Health Services and an associate professor at New York University’s College of Global Public Health.
The first case of monkeypox behind bars was reported in Chicago this week, and health experts are warning that jails could accelerate the spread as they are dangerously unprepared to combat against a virus that spreads through close physical contact. We speak with Dr. Homer Venters, the former chief medical officer for New York City’s Correctional Health Services, whose new op-ed for The Hill is headlined ”CDC must act to prevent monkeypox explosion in prisons.”
Transcript
AMY GOODMAN: We move from heat waves to the issue of monkeypox, yes, to the spread of monkeypox behind bars. On Thursday, New York’s health commissioner declared monkeypox an imminent threat to public health amidst rising concern about increasing cases in the state and elsewhere. Monkeypox can be transmitted by close physical contact, and experts say it can also spread inside households and through contact while dancing or cuddling, or by sharing contaminated clothes or bedding, or even breathing the air. Symptoms include swollen lymph nodes, fever and muscle aches, and a bumpy rash with lesions that can last two to four weeks — painful, painful lesions.
This comes as the first case of monkeypox behind bars was reported in Chicago this week at the Cook County Jail.
We’re going to continue now with Dr. Homer Venters, a physician and former chief medical officer for New York City’s Correctional Health Services. He has just written a new op-ed for The Hill that’s headlined ”CDC must act to prevent monkeypox explosion in prisons.”
Dr. Venters, we last spoke to you about the COVID-19 pandemic in the prisons. Now talk about monkeypox. While you formerly were head of health services at New York City’s Correctional Health Services, we are now talking to you in Virginia, where you’re investigating prisons and dealing with monkeypox.
DR. HOMER VENTERS: Yeah. I should say, where I am now, there aren’t any cases. But I think that my concern around the country is that there are so many places, especially the intake pens, the court pens, solitary confinement, where people are doubled or tripled up in cells, where there is a mandated, forced close contact between humans that involves skin-to-skin contact, that if you looked at the part of the CDC recommendations that deal with raves and parties and social gatherings, if you had one iota of experience or even talked to a single incarcerated person, you would realize that same contact is happening thousands — tens of thousands of times every day in jails and prisons. I am worried that — you know, right now we have about 5,000 cases reported in this country — that that number could dramatically increase, and the whole epidemiology of the American outbreak could shift in a direction that involves many more cases among people who have justice involvement.
AMY GOODMAN: So, let’s talk about the monkeypox vaccine, TPOXX. I mean, the U.S. had the foresight to store millions — right? — of these TPOXX vaccines, which dealt with — and you can explain all of this — smallpox. What happened? Why are people lined up — this is outside of prisons — trying to get this vaccine and can’t get it now, not to mention what’s happening in prisons?
DR. HOMER VENTERS: Well, I think that, you know, even what you could see in New York City, my concern is that we’re going to go down the same path of a real lack of equity in who gets access to these vaccines. Inside prisons and jails and detention centers, one of my concerns is that there won’t be adequate contact tracing to determine who, just in the post-exposure scenario, should be offered the vaccine. There will be, obviously, issues with trying to get access to vaccine for carceral settings, that are always at the bottom of the list. But just this one technical tool of contact tracing, I found through about 40 or 50 COVID inspections, often jails and prisons just don’t do it. They just don’t try and figure out who were the close contacts for these cases.
Now, monkeypox, we would assume there will be fewer cases, even when it gets into a facility. So we probably won’t have 70, 80% of everybody in a prison getting it. We may have a smaller number of people. But it still requires a will to go find out who were the people who were in that court pen, that intake pen, that housing area. And that’s where I have a lot of concern about just identifying who could, in a post-exposure scenario, be eligible. And then, obviously, there are people who are highly vulnerable that we know about today who should be eligible in a preventive or pre-exposure format.
AMY GOODMAN: So, there is something like 21,000-plus believed to be monkeypox cases in the world. Once again, like COVID, the U.S. has, what, something like a quarter of those cases, 5,000 cases. And then you have the prison population. Latinx and Black Americans make up a disproportionate share of the cases of monkeypox in the United States. And then, within prisons, the Black and Latinx population is overwhelmingly, disproportionately represented. So what does that mean inside prisons?
DR. HOMER VENTERS: Well, this means that mass incarceration is one of the ways — obviously not the only way, but one of the ways — in which we have a system that produces inequity in all levels of health outcomes. And here, we’re talking about infections. You know, the CDC and state departments of health have been essentially absent from both surveilling the health of people who are behind bars, but also promoting better healthcare for them, better health outcomes.
And a lot of this comes down to a reluctance to measure the risk of incarceration. So, Keri was just talking about it. Incarceration creates health risks to individuals and to the communities and families around the places where people are held. And so, here, it’s infections. But, you know, the same could be said for sexual abuse. The same could be said for traumatic brain injury, where people sustain them behind bars. They go home with new traumatic brain injuries. But you don’t see the CDC measuring or intervening in this health problem the way they do with youth sports or with other health problems.
So, I fear we’re down the same path. We may get some quick, fleeting involvement from the CDC and state DOHs with the most acute response to monkeypox in these settings, but no real intervention to say, you know, these places create health risks. And we have to fundamentally change our approach to thinking about health and measuring the health risks at these places.
AMY GOODMAN: So, TPOXX, the smallpox vaccine, the one that can deal with monkeypox, has a major effect the minute you get it. The problem is getting it. Who are the lobbyists to get it into the prisons, considering there’s such an overwhelmingly — there’s such a shortage of it in the United States overall? And then, what — just tick off what are the most important actions the CDC and this country should take to ensure the health of the prison population.
DR. HOMER VENTERS: Sure. So, we do have — because about a year and a half or two years ago we went through this same set of discussions around the COVID vaccine, we do have advocates, legal aid organizations, some parts of the public health structure in this country, that are ready and are thinking about access to vaccines for incarcerated people. And so, there, I think, the pump was primed — even though we didn’t get great outcomes always — with the need to go to governor’s offices, to go to state departments of health and force these questions about access. So I think we’re actually in a better spot than we would have been without COVID.
I think the CDC today needs to come up with — and I know they’re working on it — guidelines for detention settings specific to them. But they need to be much more explicit. So, these intake pens, where you cram people together, where you’re going to have transmission, they need to say explicitly, “You shouldn’t do this.” You shouldn’t be putting 40 people into a small pen, having them sleep on the floor. They should also be explicit about things they avoided talking about before, like copays should be eliminated. People who have symptoms don’t report them either because they have to pay money when they report these symptoms, especially in prisons, or they may go to a punitive setting. They may go to solitary confinement, essentially. And so, the CDC can be much more explicit.
To do this, though, their guidelines have to be much more rooted in the actual experience of incarcerated people. So they need to talk to incarcerated people. When they go to a tour, just like a state DOH, they can’t walk in and take a manicured tour from jail administrators. They need to sit down and have confidential discussions with people who are living this experience.
AMY GOODMAN: How many prisons and jails in this country?
DR. HOMER VENTERS: We have 3,000 jails, about 2,000 prisons, and another 2,000 juvenile detention and immigration centers, so about 7,000 of these boxes. So, if you think we have 5,000 cases in this country today, that number can dramatically increase, and —
AMY GOODMAN: We have to leave it there. And I want to thank you, Dr. Homer Venters, for being with us.
DR. HOMER VENTERS: Thanks, Amy.
AMY GOODMAN: The former chief medical officer for New York City’s Correctional Health Services. I’m Amy Goodman. Thanks for joining us.










Media Options