
Inequality in the U.S. medical billing system leaves the uninsured paying far more for medical care than those with insurance. We speak with a patient who was uninsured when she received an emergency appendectomy and was charged five times higher than what Medicaid would have paid and others including the Legal Aid Society’s Elisabeth Benjamin author of the report, “State Secret” which finds New York City hospitals aren’t informing patients about available state government charity funds. [includes transcript]
Today we take a look at the state of health care in the U.S. today. In November, the Senate narrowly approved President Bush’s package to overhaul Medicare. And in the run up to the 2004 presidential election, health care is one of the main points of contention as Democratic presidential candidates hotly debate the issue on national TV.
Well today we are going to take a look at the people who don’t have health care in America. Rising costs of new procedures and drugs as well as deregulation of the industry has sent charges at virtually all hospitals across the county soaring.
Who is to pay for these rising prices?
Well, the widespread practice among hospitals is that the uninsured are expected to pay far more for their medical care than large insurers, HMOs or even the U.S. government.
In other words, there is a major inequality in the billing system: The poorest patients are billed at prices many times higher than what insured people are charged for the same treatment.
Hospitals negotiate discounts with big institutions such as insurance companies or the government that require payment of only a fraction of the listed charges. These institutions have strong bargaining power and can guarantee hospitals a certain number of patients.
Uninsured patients, on the other hand, have no bargaining power and aren’t even told that big institutions get these reduced rates. As a result they end up with huge medical bills and no way of paying them.
Hospitals then hound those patients for payment using collection agencies and lawyers who use such methods as filing lawsuits, slapping liens on homes, seizing bank accounts, and garnishing wages to extract payment.
Part of the reason the uninsured cannot pay their medical bills is because hospitals aren’t informing them about available resources and charity care.
For example, a few states operate a funding pool for hospitals to offset the money they spend on charity care as well as their bad debt. The total amount of money in the pool in New York State is approximately $847 million a year.
Today we will begin by taking a look at New York City. A Legal Aid Society study of 22 hospitals citywide titled “State Secret” finds that hospitals have failed to develop a process that would let poor and uninsured patients apply for state government funds to help pay for their hospital care.
- Jennifer Kankiewicz, was rushed to Beth Israel hospital in July 2002 for an emergency appendectomy and was hospitalized for two days. The total cost she was billed for was over $23,000. Her current bill stands at over $19,000–more than her annual salary.
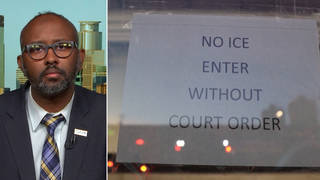
- Elisabeth Benjamin, supervising attorney of the Health Law Unit of The Legal Aid Society. She is the author of the new report “State Secret: How Government Fails To Ensure That Uninsured And Underinsured Patients Have Access To State Charity Funds.” [Download pdf file]
- Raymond Sweeney, executive vice president of the Healthcare Association of New York State.
- Mark Rukavina, executive director of the Access Project, a Boston-based research group that focuses on health care and the uninsured.
Transcript
AMY GOODMAN: We’e joined today by Jennifer Kankiewicz who was rushed to Beth Israel hospital in July for an emergency appendectomy. We are also joined by Elizabeth Benjamin, who is supervising attorney for the Health Law Unit of the Legal Aid Society and author of the new report, State Secret–How the Government Fails to Ensure that Uninsured and Underinsured have Access to State Charity Funds. We welcome you both to Democracy Now! Jennifer Kankiewicz, lets begin with your story. Tell us what happens in July.
JENNIFER KANKIEWICZ: Overnight I got terribly ill. I waited through a day’s worth of not being able to get out of bed because I didn’t have health insurance. The next day, a friend drove me to the hospital in an emergency. And we went to the closest hospital we knew of.
AMY GOODMAN: Which was?
JENNIFER KANKIEWICZ: Beth Israel.
AMY GOODMAN: And what happened? Did you have an appendectomy?
JENNIFER KANKIEWICZ: Yes. They provided great service. I had an appendectomy, and they reassured me that I could apply for Medicaid assistance. So, maybe Medicaid would help me with the $24,000 that it cost me.
AMY GOODMAN: And what happened afterwards?
JENNIFER KANKIEWICZ: Medicaid was denied. I put forth an appeal myself, and went to a fair hearing. I was able to reapply, but you know, unless I–either disabled or pregnant, I could not possibly qualify for Medicaid.
AMY GOODMAN: Why couldn’t you qualify for Medicaid?
JENNIFER KANKIEWICZ: I believe the rate is $350 a month. You must earn that or less to qualify.
AMY GOODMAN: Okay.
JENNIFER KANKIEWICZ: It would be very difficult for me to exist in New York City and pay my rent and to live on those wages.
AMY GOODMAN: You didn’t qualify for Medicaid, but the bill for the appendectomy was?
JENNIFER KANKIEWICZ: I actually billed by six different billing groups. Beth Israel’s bill was $19,488, but the surgeon and the anesthesiologist, the radiologist, they all bill separately.
AMY GOODMAN: In addition?
JENNIFER KANKIEWICZ: Exactly.
AMY GOODMAN: It’ swell over $20,000.
JENNIFER KANKIEWICZ: Total bill was $25,000 but I was able to negotiate little bits with some of the other billing groups. My surgeon cut significant portion of my bill, but Beth Israel was not able to discount me unless I was able to pay all of the bill up front.
AMY GOODMAN: You couldn’t?
JENNIFER KANKIEWICZ: No, no, no. I don’t have much of a savings. I kind of–you know, I work hard, but I kind of live check to check sometimes.
AMY GOODMAN: Elizabeth Benjamin, you are the supervising attorney at the health law unit of Legal Aid Society. How typical is Jennifer? story?
ELIZABETH BENJAMIN: Unfortunately, Jennifer? story walks into our office every single week. We have been inundated with client after client after client people who are underinsured or uninsured who have no ability to pay these jacked up rates. Jennifer, for example, if she had been insured for Medicaid and she’s absolutely right. To be eligible for Medicaid, you cannot earn a penny more than $350 a month in New York state, unless you are disabled or pregnant. If Jennifer had Medicaid, her bill would have been $5,000. So?
AMY GOODMAN: Wait.
ELIZABETH BENJAMIN: Yeah. Medicaid only pays Beth Israel $5,000 for an appendectomy. That? a 500% markup that Beth Israel is doing on the backs of the uninsured. Beth Israel, I mean I don’t want to pick on Beth Israel, they all do it. For example, a Flora Alba Guzman a client of ours in Queens earns only $7,800 a year as a housekeeper. She goes from home to home, she is only Spanish speaking. She was rushed for a heart condition to MT. Sinai hospital and her bill was $12,000. On top of that, she was asked to pay $1,000 to fund New York state pool for the uninsured, that each one of these hospitals get lots of money for, supposedly to take care of the uninsured. So, for example, in Jennifer? case, Beth Israel gets $28 million a year, on average, to take care of uninsured patients like Jennifer, but they didn’t offer that program to Jennifer.
AMY GOODMAN: Was there some kind of application that you could have filled out?
JENNIFER KANKIEWICZ: After I was denied Medicaid, I went back to financial assistance at Beth Israel. They weren’t able to offer me any options. They said that I should wait until the bills are consolidated in collections then I would be able to negotiate with collections a payment plan.
ELIZABETH BENJAMIN: That’s like sending her out–it’s like sending a little guppy out to the sharks. It? just not fair. We have patient after patient who come where they have been sued. They don’t know they have been sued because the collection attorneys and the collection agents hired by the hospitals are voracious. They serve people. They claim to serve people, but in fact they have never served any body with court papers. The next thing my clients know, their bank accounts have been taken.
AMY GOODMAN: Well, we did try to get Beth Israel on the phone. They said your Medicaid had been denied but they didn’t come on the telephone. We do, however, have Raymond Sweeney, Executive Vice President of the Health Care Association of New York State, otherwise known as H.A.N.Y.S. What about this case? On the one hand, you have a young woman who faces a bill of close to $20,000 for an appendectomy and on top of that we find out that she is being charged something like four to five times what people would be charged if they had Medicaid or they were insured.
RAYMOND SWEENEY: Well, I don’t know the specifics of the case. I heard the description. Usually the markups in New York actually are less than around some of the rest of the country, an average of around 100% as a markup. What happened to Jennifer shouldn’t have happened. I think the short answer is we have to do a better job communicating up front with patients that are low income and can’t afford to pay their bill to do a better job explaining that financial assistance is available.
AMY GOODMAN: But is financial assistance available? Is there actually an application that someone in the hospital who is more educated could have given her?
RAYMOND SWEENEY: We tried to collect. This is, as your lead-in suggested, this has been reviewed and being discussed around the country, going back, 6 to 9 months now and we started ourselves as an association in June to collect policies from various institutions. I don’t know if we have one from Beth Israel or not. Frankly, but we have had 30 or 40 from around the state and the one difference from the work that Elizabeth Benjamin did in Legal Aid in New York City is we found lots of policies. We have collected 30 or 40 of them and virtually all of them had income scales, eligibility scales and discounts available for individuals for in-patient care such as the services Jennifer received. But honestly, what we found also is that it wasn’t easily communicated, that it wasn’t available or posted adequately, that patients haven’t been informed consistently enough that this kind of assistance is available, and that’s the thing we need to correct, and that’s what we are going to work on. The one quarrel that I would have with your setup on this, in particular in New York City, hospitals deliver, really, care–free care to 3 million people who are uninsured, as is Jennifer. She? one of 3 million in New York. There isn’t another sector that in effect provides services for free, because health care unique and we have to do that. We do it, but we have to do it by adding up the income from governmental payers and private payers, and somewhere, if we want to have the system available to provide those services, the sum of the parts have to add up to the whole, and they don’t. They don’t in New York. They fall short even with all of the assistance, government and the state provides.
AMY GOODMAN: Let me ask Elizabeth Benjamin who did this report, ?tate Secret–How government fails to ensure that uninsured and underinsured patients have access to state charity funds.?Can you tell us how did you the study, which hospitals you went to, which said have an application and which said they didn’t?
ELIZABETH BENJAMIN: What we wanted to do was figure out how the $847 million is spent in New York state, in New York City. Frankly, we really thought we would find exactly what Ray is describing. We thought we would go to the hospitals and end up with a rather complicated consumer booklet that explained each hospital’s policy. What we didn’t expect to find, but what we did find is that at all 22 hospitals we surveyed, not one of them had a charity care program where an insured patient could apply for the funding. Each one of those hospitals got anywhere from $4 million to $60 million in charity care funds from the state, supposedly to take care of bad debt and charity care losses that they suffer. Ray is right. We have a huge uninsured problem in New York state. What we did, the way we tried to find it out and no hospital has quote, unquote, corrected the record with us. It seems in some ways we were accurate in the sense that we went, we first called the hospitals three times. We found very little by calling. An average consumer that might want to call a hospital and find out what the charity care policy is, forget it. We then physically went to the hospital. Some patients accounts offices were more than 15-20 minutes walk away from the main hospital. We had to ferret them out, but in fact at all 22 hospital, that at least would speak to us, we found their billing offices. We went to the billing offices and we talked to them. What we found was that at all 22, no one had a way to actually get the state money applied to your case. So, for example, Beth Israel, which is one of the hospitals that we surveyed, has no way to provide funds, these bad debt and charity funds, the $28 million they get a year to Jennifer? case. That? fine. What the hospitals then do is make people like Jennifer, who are absolutely not eligible. I could have told Jennifer in 30 seconds, she wasn’t going to be eligible for Medicaid. They make them go through this process of applying for Medicaid. I don’t mind that they make my clients goes through the process of applying for Medicaid, but it is in some cases a futile exercise. For her to have gone to a fair hearing on her own was just a waste of time. Then we thought, okay, so maybe the people at the front desk in the billing offices or their supervisors who we also asked to speak to, don’t know so much, so we’ll write the lawyers and the heads of the hospitals on individual cases like Flora Alba Guzman, the woman who was the housekeeper who has $7,800 in income but has a $12,000 bill for not even a an overnight stay at Mt. Sinai hospital. We will write to the hospitals and their lawyers, we sent them certified return receipt to make sure they got the letters, saying that, couldn’t you apply some of these funds to Ms. Guzman’s case? None of them replied. Then we decided, let’s find out what the charges are going to be. We called the hospitals and found out the charges. They were all over the place. It ranged from $1,500 to $11,000 for an overnight hysterectomy. So the fact is that you as an uninsured consumer have no capacity to find out what the programs are. The programs at least for allocating charity care in New York City don’t exist, at least at the 22 hospitals we went to. There are 60 hospitals in New York City. We couldn’t go to all 60. I think 22 is a good effort. The bottom line is they aren’t required to. The government gives them money, to the hospitals.
AMY GOODMAN: This is the state legislature.
ELIZABETH BENJAMIN: The state legislature. They give these hospitals nearly $1 billion unfettered. They don’t have to set up programs for the uninsured. There doesn’t have to be an application. There is not anything like everybody under 200% of poverty should only be charged the Medicaid rate, which is exactly the cost for providing the care. There is no rules protecting the patients. The only rule that they do have is that they must pursue the patients vigorously. So in fact the government encourages the hospitals to aggressively chase them.
AMY GOODMAN: Well, we have to break for stations to identify themselves. When we come back, we will continue this discussion. We’e also going to be speaking to a man in Illinois, who was jailed because he could not fully pay his hospital bill. The question is, are we returning to debtor’s prisons in this country? Stay with us.
AMY GOODMAN: We look at the state of health care in America, but specifically the issue of the uninsured in this country being charged as much as five times the rate as someone who is insured or someone who has Medicaid. Joining us in our studio, Jennifer Kankowicz who was rushed to Beth Israel Hospital in New York City for an emergency appendectomy and hospitalized for two days. She faces a $20,000 hospital bill. Elizabeth Benjamin who did a ground breaking report, this applying to New York, called State Secret, How Government Fails To Insure That Underinsured and Uninsured Have Access to State Charity Funds. Raymond Sweeney is on the phone with us from Albany. He’s Executive Vice President of the Health Care Association of New York State. And we are also joined, as we take this story national, by Mark Rukavina, who is Executive Director of The Access Project, a Boston based research group that focuses on health care and the uninsured. Mark, can you tell us, is Jennifer’s case unusual in the country? We know it’s not unusual in New York City.
MARK RUKAVINA: No, it’s unfortunately not unusual in the country. We are seeing in many communities that uninsured people are — the good news for uninsured people is they’re able to access health care, but the bad news is they’re left with lingering medical debt that does them harm in many ways. We have done some studies that indicate that people are reluctant to go back to providers if they owe them money. And, you know, what we’re we’re seeing here is a real crisis, since the uninsured, as you said, pay at the highest rates. We have worked in many states, and have a very difficult time, similar to the study in New York — uninsured people, groups that work with uninsured people, have an extremely difficult time getting information on programs that are in fact designed to serve uninsured patients.
AMY GOODMAN: Now, it sounds, Elizabeth Benjamin of the Health Law Project of Legal Aid Society, that New York was different from, for example, New Jersey, Connecticut, Massachusetts, in that they do not in fact have an application. It’s not that the secretary couldn’t find the application. There was no way to apply for this.
ELIZABETH BENJAMIN: Right. New York state, as far as I know, is the only state that allocates as much as $1 billion to the hospitals with no strings attached. In — we have a client from New Jersey. He had charity care forms that he could apply for for his daughter with a cleft palate, but when his wife had terminal cancer and came to Our Lady of Mercy in the Bronx, there was no charity care for him. He asked where was the charity care, and they said, we have no charity care, even though they get $9 million a year to provide charity care. Massachusetts has a charity care program, by statute. Connecticut, after the scandal that erupted there last year, now has a charity care statute. Even Washington state, which has no funds for their charity care program, has a mandatory requirement for every hospital to provide charity care application.
AMY GOODMAN: You referred to a scandal in Connecticut. What happened?
ELIZABETH BENJAMIN: In Connecticut, actually the union there, 1199, and a bunch of consumer advocates got together and exposed how Yale New Haven Hospital, you know, charged these crazy rates but were also taking liens on their patients’, low income patients’, homes. In fact one of the patients, a gentleman, was profiled in the “Wall Street Journal”. He had been paying his wife’s who died 20 years before — his wife’s debt off for years now, and had no hope of ever getting out from the debt.
AMY GOODMAN: So what happened? How much had he paid?
ELIZABETH BENJAMIN: He had paid, I believe, $16,000 altogether, and still owed much, much more. And what they do, and they do this in New York state, for example, the collection agents charge 9% interest. So, even though the federal interest rate is 1%, and most people can get mortgages for 6%, the hospital industry is charging 9%, at least, you know, on average in New York state.
AMY GOODMAN: so, you could be paying partially your bill, but it would still go up — continue to go up every year.
ELIZABETH BENJAMIN: Yes. We have that case many times.
AMY GOODMAN: Let me ask Ray Sweeney from the Hospital Association of New York state, why is New York unusual and not even providing applications? People don’t even have the chance to cut these bills that they’re getting, that are so much higher than those who are insured or who have medicaid?
RAY SWEENEY: Thank you. I was going to jump in. I think we are mixing two different things. New York does provide a substantial amount of aid for the hospitals that provide free care to people, and actually was the first in the country to do so, and has done the most to make sure that services are available and open to people who can’t afford to pay, and who are uninsured. But it’s disconnected from an individual applying for it. It’s simply the nearly a billion dollars that’s made available is — covers around 50% of the total of free care, most of which is downstate in New York City. The free care that’s actually delivered. So, it’s not made available on a patient by patient basis, because it doesn’t go anywhere near far enough to pay for the level of care, not inflated care just the level of care that’s really being provided to people. And if we went through a process like New Jersey and Massachusetts, I think, does, with an individual application process, we would certainly enrich billing offices and accounting firms, but we really wouldn’t be solving the problem of providing affordable health care to individuals. That doesn’t mean that on an individual hospital by hospital basis people shouldn’t have financial assistance available, shouldn’t have clearly articulated eligibility for financial aid.
AMY GOODMAN: Elizabeth Benjamin, your response.
RAY SWEENEY: Sliding scales that are available, discounts available to people who really cannot afford to pay, those are obligations that institutions should have. And again, when we tried to collect policies, we found lots of hospitals, most hospitals, actually having those policies, not necessarily implementing this as consistently as they should.
ELIZABETH BENJAMIN: I think, Ray reached out to the hospitals, and the hospitals who responded to Ray’s effort, which I laud, were the ones that do have policies to show him. The problem is, at least downstate, the hospitals’ policies don’t really exist, and we know that for sure. The bigger problem, however, is this, which is that all of our neighboring states have this application form. Ray is saying, look, we’re only getting paid 50 cents on the dollar, but that 50 cents on the dollar is not coming back to the uninsured patient. The patient never knows that the hospital has been paid for their debt. So, Ray’s hospitals are collecting — not Ray’s hospitals, but the state, the city hospitals are collecting money on Jennifer, and people like Jennifer’s debt, but she is never informed that it’s been covered.
AMY GOODMAN: Ray Sweeney, could you explain that? They’re paying for her care, but she’s also being told she has to pay, for, not just for the care but five times what perhaps someone else would pay if they were insured for that very same appendectomy.
RAY SWEENEY: Well, again, it’s —- the people get paid based on the free care they delivered actually two years ago, because it takes that long to collect the information and for the state to distribute the dollars. So, it’s not done on a current time basis or on a current individual patient by patient basis, and that would add tremendously to the administrative costs without any value, I think. There’s not enough money. You started by talking about the cost of health care in the system, the fact that every payer is trying to find the least they can pay for services rendered, and yet we still have 15% or more of the population who are uninsured. -—
ELIZABETH BENJAMIN: I’m glad Ray raised the issue about the uninsured, because we actually took the money, we took the 847 and divided it by the number of how much it would cost to insure people with the state low income insurance program. And it would cover 228,000 people. So, those 228,000 people would know that they have health care. Right now, no one the uninsured do not benefit from the system. The hospitals get 50 cents on the dollars they have expended, but the uninsured get nothing and that’s the problem.
MARK RACOVINA: Amy —
AMY GOODMAN: Mark Racovina, of the Access Project in Boston.
MARK RACOVINA: I’d like to jump in here. I think New York state is unique. It’s one of the states that does provide hospitals for some of the uncompensated care, but I’d like to bring this back to Jennifer’s story and what happens to uninsured patients when they do receive care. And what happens is they are billed at the highest rates, and that is simply wrong. They should also enjoy the benefits that people in Blue Cross plans or other insurance plans receive, because hospitals provide those patients with discounts. We believe that hospitals could provide similar discounts to uninsured patients, the vast majority of whom are having a difficult time paying for these hospital bills. What we have found in community after community where we have done this work is that uninsured patients fully intended to pay their bills, until they received the bill, and had to face that sticker shock when they realized just how expensive these services were, or — or I should say, what they were charged for the services.
AMY GOODMAN: Jennifer —
MARK RACOVINA: You have heard about the discrepancy between what Jennifer was charged and what others are charged —
JENNIFER KANKOWICZ: I’m sorry to interrupt. I just wanted to explain that I’m not looking for a free ride. I really want to compensate Beth Israel because I got excellent care and they saved my life, but I paid $3,150 for every overnight, even though one of those nights was six hours on a gurney bed. And, I want to pay them, but it is just unreasonable.
AMY GOODMAN: Ray Sweeney.
RAY SWEENEY: Yeah, I appreciate that, and I appreciate that individuals, as we have talked to uninsured patients as well, want to do as much as they can to pay for services rendered. I should say, and I don’t know if you reached out to the American Hospital Association, but in December, the American Hospital Association issued a set of guidelines to all hospitals nationally. We’re working on something ourselves in New York that go perhaps a little bit beyond that, but we’re not yet through with the process. But it addresses all of what you have been talking about, that hospitals should be, they have an obligation and we ought to be doing a better job (muttering)–that we need to do a better job and recognize that and we’re prepared to do that.
MARK RACOVINA: And Ray is right. And we have been in contact and we have been in communication and have met with the American Hospital Association on their guidelines. We applied them for this work. And their guidelines are quite straightforward. They say that they’re encouraging their members to make public and available the charges for their services so that Jennifer knows when going into the medical setting what something is going to cost her and people like Jennifer, that they review their current charges to insure that they’re reasonably related to both the costs of the services and to meeting all of the community’s health care needs. They also encourage the members to provide financial counseling to patients about their hospital bills.
AMY GOODMAN: Jennifer let me just ask —
MARK RACOVINA: And have understandable written policies to help people, these uninsured patients, determine whether or not they qualify for either public assistance or some kind of hospital bill program.
AMY GOODMAN: Let me ask Jennifer a question, since she can’t qualify for Medicaid. What would you have done when you had this appendicitis attack, if you had been given the chance to evaluate the finances?
JENNIFER KANKOWICZ: Well, actually —- I’m so uneducated about this. When I eventually spoke to Beth Israel collections, the woman there said, why did I choose the most expensive hospital, if I’m uninsured? Honestly, I didn’t understand that. I was a consumer that had to shop. I didn’t realize there was a discrepancy between hospital costs, and -—
AMY GOODMAN: How did you choose Beth Israel?
JENNIFER KANKOWICZ: I wasn’t making a decision at the time. I rushed to the hospital. I knew where that was, I used to live nearby, and I kept explaining to them, I don’t have insurance, and they said, I could apply for Medicaid, and I was reassured. I don’t know what else I could have done.
AMY GOODMAN: I want to go to another issue right now, as we look around the country at various policies. We’re going to go to Illinois to Claudia Lenhoff, who is the Executive Director of the Champagne County Health Care in Illinois. As we read through the different articles, and the research on what people are facing in the country, Illinois definitely stood out around the issue of body attachment. Can you explain what this is?
CLAUDIA LENHOFF: Yes. Body Attachment is basically a warrant for arrest, and in our state, it’s just called a Body Attachment, and it is literally where, through a court proceeding — usually what happens is that if somebody misses a court date, or fails to appear for some reason — in our case, what happens is that the hospital attorney, you know, when the judge asks the hospital attorney what would you like to do, how would you like to proceed, hospital attorneys have an option of rescheduling the hearing or doing any number of things, but in our community, our hospitals have been requesting Body Attachments. And that’s basically where they’re requesting that t









Media Options