
Topics
Guests
- Dr. Homer Ventersphysician and the former chief medical officer for New York City’s Correctional Health Services. His new book is titled Life and Death in Rikers Island.
- Jennifer Gonnermanstaff writer for The New Yorker magazine. Her most recent piece is titled “Do Jails Kill People?”
The former chief medical officer of New York City jails has just published a remarkable new book about the health risks of incarceration. The book is titled “Life and Death in Rikers Island.” Dr. Homer Venters offers unprecedented insight into what happens inside prison walls to create new health risks for incarcerated men and women, including neglect, blocked access to care, physical and sexual violence, and brutality by corrections officers. Venters further reveals that when prisoners become ill, are injured or even die in custody, the facts of the incident are often obscured. We speak to Dr. Venters and Jennifer Gonnerman, staff writer for The New Yorker magazine.
Transcript
AMY GOODMAN: This is Democracy Now! I’m Amy Goodman. His name is synonymous with all that’s wrong with the prison system: Kalief Browder. Kalief spent three years at Rikers Island jail in New York without charge. He was a 16-year-old high school sophomore when he was detained on suspicion of stealing a backpack. Browder never pleaded guilty, was never convicted. He maintained his innocence and requested a trial, but was only offered plea deals while the trial was repeatedly delayed. He was held at Rikers Island jail for three years, beaten by guards and prisoners alike. After enduring nearly 800 days in solitary confinement and abuses, Browder was only released when the case was dismissed. He committed suicide on June 6, 2015, at his home in the Bronx. He was 22 years old. Nearly four years later, the question remains: Why did Kalief have to die? Is there something inherently wrong with incarceration that makes it a health risk, sometimes with deadly consequences?
Well, a remarkable new book attempts to answer those questions as it shines a light on the health risks of imprisonment. The book is titled Life and Death in Rikers Island. Its author, Dr. Homer Venters, the former chief medical officer of New York City jails. He offers unprecedented insight into what happens inside prison walls to create new health risks for incarcerated men and women, including neglect, blocked access to care, physical and sexual violence, and brutality by corrections officers. Venters further reveals that when prisoners become ill or injured, or even die in custody, the facts of the incident are often obscured. He writes, quote, “[W]e work in settings that are designed and operated to keep the truth hidden. Detainees are beaten and threatened to prevent them from telling the truth about how they are injured, health staff are pressured to lie or omit details in their own documentation, and families experience systematic abuse and humiliation during the visitation process,” unquote. The risks of jail are disproportionately harmful for people with behavioral health problems and for people of color, Venters explains. He concludes Rikers Island must close, and suggests how that should be done.
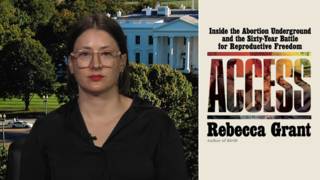
Well, Dr. Homer Venters joins us now, physician and former chief medical officer for New York City’s Correctional Health Services. Again, his book, Life and Death in Rikers Island. He’s currently senior health and justice fellow at Community Oriented Correctional Health Services and associate professor at New York University’s College of Global Public Health. Also with us, Jennifer Gonnerman, staff writer for The New Yorker magazine. Her most recent piece is a review of Dr. Venters’ book. It’s called Life and Death in Rikers Island. “Do Jails Kill People?” is the name of her article.
Welcome you both to Democracy Now! OK, Dr. Venters, start off talking about why you wrote this book and how Kalief Browder’s death relates to all of this.
DR. HOMER VENTERS: Well, early on in my time overseeing the health system in the New York City jails, it became clear that our job was not just to take care of people who were injured or address the medical problems people had, but that this system was conferring new health risks to our patients. So, our patients were getting hurt because of the way the jails were set up and run. And so, it was clear to my team and I that part of our mission had to be to use our tools as public health and epidemiology folks, as well as doctors and nurses, to document just what these health risks were and to report those out. And one of the things that over the years became clear is that those health risks, as you just stated, aren’t meted out in a uniform fashion. People with behavioral health problems, people of color, our data show, were more likely to find themselves on the wrong end of these health risks.
AMY GOODMAN: Talk about why prisons are lethal. Talk about Rikers Island, for example.
DR. HOMER VENTERS: Well, we can start with the first and most serious health risk, which is death. It’s clear that there are many preventable, or what we would call jail-attributable, deaths that happen. We worked hard to document those while I was leading the health service in the New York City jails, but there are many others. So, for instance, people that we know who are coming in with very serious health problems—diabetes or hepatitis C or needing dialysis—who then are denied those services, despite the fact that we have them available; people who are exposed to solitary confinement, not just the isolation, but the brutality and violence associated with it, who do take extreme measures to get away from the distress that that setting causes—those are things that were conferred to those people.
AMY GOODMAN: Tell us the story of Carlos Mercado and Angel Ramirez.
DR. HOMER VENTERS: So, those are two patients who, as have been publicly reported, entered into the jail system with clearly identified health problems, one with diabetes and one undergoing withdrawal. And as has been reported in the press, they both, despite having clearly communicated their problems and even having their problems elicited and understood by quite a few people in the jails, received a punishment response and a neglect response that led to their death, even though they were in a system that was able to provide them the healthcare they needed.
AMY GOODMAN: So what happens to a prisoner when they’re sick? You also talk about the tension between the doctors, the nurses—the health professionals—and the guards.
DR. HOMER VENTERS: In the best of circumstances, the correctional officers, who are with our patients all the time—you know, they see and interact with people much more than we do in the health service—they determine that somebody is ill and they need help, or somebody just reports, “I don’t feel well,” then they’re taken to medical care, and they get the appropriate level of medical care. They’re transferred to the hospital if they need something that the jails can’t provide.
In the worst circumstance—and there are some situations that actually hardwire in this less ideal response—people aren’t able to say that they’re sick or that they feel well, or when they do, they’re not believed, and so they’re kept in a chaotic intake pen, or they’re kept in a solitary confinement cell, even though they’re saying, clearly, “I need insulin,” or “I’m sick,” or “I’ve just swallowed something that could kill me,” and then they’re denied access to healthcare.
And then, finally, I would say that because of the pressure of dual loyalty, this really crushing and very omnipresent ethical problem, human rights problem, in correctional health, that even when they do make it to the health service, sometimes the doctor or nurse or social worker in front of them is acting more as an agent of the security service than as a healthcare provider.
AMY GOODMAN: Talk about your own experiences. You entered the jails in what? 2008?
DR. HOMER VENTERS: Yes.
AMY GOODMAN: About a decade ago?
DR. HOMER VENTERS: Yes.
AMY GOODMAN: What did you find there? What shocked you most?
DR. HOMER VENTERS: I believe that what—one of the things that shocked me the most was the high level of injury and injury associated with violence. Certainly, all physicians and healthcare people, we have experience taking care of injuries. But so many of our patients were coming to us with injuries, and so many of them were saying that these injuries were from things called slip and falls. So, you know, patients that come with a fracture to the jaw, a very—you know, very serious injury, or a fracture of the upper arm or the leg, and then saying that they had slipped and fallen—things that just did not—you know, we didn’t believe. But also, it was clear, when you interacted with these patients, that they were terrified and that they, actually, in that moment, were thinking very clearly about their survival and their preservation. And so, it makes a very difficult proposition for a doctor or nurse.
AMY GOODMAN: So, you set up an injury surveillance system?
DR. HOMER VENTERS: That’s right. Shortly before I arrived, Christopher Robinson, another young man who died in that same jail that Kalief Browder was held in, he had been beaten to death. And so, when I did arrive and started with the Correctional Health Service, we set about understanding how many other people were injured, especially adolescents. And we saw lots of jaw fractures and hand fractures. And so, at first we were dealing with paper records, but then we quickly implemented in the New York City jail system an electronic medical record. But we were able to modify that in really major ways, so that we could capture data not just about the type of injury people had, but about whether or not it was intentional. Did it happen during a use of force? Was there a blow to the head? Then we could use that data to report out to others, not just in the correctional service or the city, but outside parties that might be interested, what the rates of injury were, so that we had empirical data to show that brutality and injury was in fact a real crisis for our patients.
AMY GOODMAN: Describe what would happen when you would send an email to the DOC, to the Department of Corrections, to upgrade an injury, to upgrade what you saw.
DR. HOMER VENTERS: Well, the injury reporting system on the health side, as I mentioned, we built a pretty sophisticated electronic medical record system. On the security side, it required paper, pieces of paper, injury reports, to be updated and amended actually on an individual piece of paper. So, when I would find a patient, as I often would, who had an injury that was more serious than initially reported, or that the circumstances of the injury were different than was originally reported, unlike in healthcare, where we want all information to lead us to the quickest, best outcome for the patient, these paper forms then would be put back in my face, and people would say, “Listen, you have to find the original doctor or go to the original jail. Go find this piece of paper”—that nobody can find. “That’s the proper way to get this addressed, not simply to tell us that, just because you’re a doctor or a health administrator, you think something else happened.”
AMY GOODMAN: Why is there so little transparency? Talk about the silent complicity you describe.
DR. HOMER VENTERS: You know, these are paramilitary settings. And so, the health service, in most of these places, even when we have an independent health authority, we still rely on the correctional staff for our safety and security. And so, as such, because there isn’t a lot of mandated transparency about health outcomes, about the true characteristics of injuries, for instance, at the time we were doing this work, most of the system is designed to keep information on the inside, so that anybody who wants to change the original account, whether it’s a patient or a doctor or a nurse, faces a real gauntlet of challenges, that not only are bureaucratic and administrative, but actually could put their own personal safety at risk.
AMY GOODMAN: We’re going to break and then come back to this discussion and bring in Jennifer Gonnerman, who wrote the review of your piece for The New Yorker—the review of your book. Dr. Homer Venters’ book is called Life and Death in Rikers Island. Stay with us.
[break]
AMY GOODMAN: “Blue Prelude” by Ethel Ennis, Baltimore’s “First Lady of Jazz.” She passed away February 17th at the age of 86. This is Democracy Now!, democracynow.org, The War and Peace Report.
I want to turn to Kalief Browder in his own words. Kalief Browder, of course, is the—well, was 16 when he was arrested and sent to Rikers Island. He ended up being there for three years, much of that time in solitary confinement, without charge. He was arrested when he was a high school sophomore. Police believed—they said that he stole a backpack, but could never come up with the person who made the accusation, who they drove around a neighbor, and the person pointed out Kalief walking on the street. And then that person just disappeared. Kalief would not plead in prison, because he said he was taught not to lie, and he said he was innocent. Held for three years, much of that time in solitary confinement. He said that while he was in solitary confinement at Rikers, the guards often refused to give him his meals.
KALIEF BROWDER: If you say anything that could tick them off any type of way, some of them, which is a lot of them, what they do is they starve you. They won’t feed you. And it’s already hard in there, because if you get the three trays that you get every day, you’re still hungry, because I guess that’s part of the punishment. So, if they starve you one tray, that could really make an impact on you. And—
MARC LAMONT HILL: How much were you starved?
KALIEF BROWDER: I was starved a lot. I can’t even—I can’t even count.
AMY GOODMAN: So, that was Kalief Browder speaking on HuffPost Live, when it was around. He died within two years after this interview. He took his own life. He went on to say he was once starved four times in a row—no breakfast, lunch, dinner or breakfast again. After enduring nearly 800 days in solitary, Browder was only released when the case was dismissed. Browder took his own life June 6, 2015, at his home in the Bronx. He was 22 years old. He was a student at Bronx Community College.
Jennifer Gonnerman wrote a lot about his case for The New Yorker and exposed videos that were gotten from the inside of Rikers showing him being beaten by guards and prisoners alike.
Jennifer, you have covered the prison system a lot. And you were really taken with this book, Life and Death in Rikers Island, and wrote a review of it for The New Yorker.
JENNIFER GONNERMAN: Yeah, you know, I saw an early copy of this book in December. And a lot of books come in. You know, as a reporter, you get a lot of—often get a lot of books and people who want publicity. I started reading this book, and I really couldn’t put it down. I thought it was so important, crucially important. And I feel like it covers one of the most overlooked aspects of mass incarceration. I mean, mass incarceration has gotten a lot of attention in recent years. But what—the health risks that folks endure when they go inside is something that I feel needs much more attention. And I think, as a society, we’ve sort of grown numb to these headlines, like an individual died in prison or jail, and we don’t really follow up with the necessary questions. And what Dr. Venters’ book does is really pushes us to ask those harder questions, like: Did this death have to happen? Was it preventable? Did something happen in the jail that led to this individual’s death? And those are the kind of questions the public—and journalists, in particular—really need to be asking.
AMY GOODMAN: Tell us the case of Ronald Spear.
JENNIFER GONNERMAN: Ronald Spear is one of the gentlemen in the book. He was in Rikers Island. He was in his fifties. He was a kidney dialysis patient. In 2012, one night, he felt very ill and tried to get the attention of the doctor. He was housed in the infirmary on Rikers Island. There was a medical office next door to his dorm. He snuck out of the dorm to get into the hall to get to the medical office, and the doctor told him—you know, a guard stopped him, and the doctor said, “You have to keep waiting.” He had been waiting for hours. The officer, the correction officer, and Mr. Spear got into an altercation, which ended with two other guards coming in and restraining him on the floor. And that would have been the end of the situation, but then the first officer, whose name is Brian Coll, came in and kicked Mr. Spear in the head repeatedly, and he died right there on the floor. This case was covered up, lied about for years, until, finally, federal prosecutors in the Southern District in Manhattan brought a prosecution against the officer. And he went on trial in 2016. So I sat through the trial. And obviously the focus was on what this officer did and didn’t do.
But one of the subtexts of that court case was what the medical staff was doing at the time. So, this crime took place in the hallway right outside the medical offices, and the nurse got on the stand and said, when she heard the altercation in the hallway, she opened her door, and then she shut her door, and that she had sort of been taught to do that. It’s almost like an unofficial rule on Rikers Island. And the doctor who was on duty and hears all of this commotion going on in the hallway, he was sitting in his office and never looked out the window, never opened the door, testified to all of this, and only opened his door after the whole thing was over, and somebody knocked on the door—I believe it was a captain—and said, “Can you come out here and, you know, help?” And at that point, Mr. Spear is on the floor, in handcuffs, face down and no pulse. And so, essentially, this homicide took place within feet of the medical staff. And that always stuck with me. And, you know, this idea of an unofficial rule of averting your eyes when there’s an altercation between correction officers and inmates is something that actually shows up in Dr. Venters’ book also.
AMY GOODMAN: You say that 112 people died in New York City jails between 2010 and 2016. That’s like almost what? Twenty a year.
JENNIFER GONNERMAN: More, probably, in some years, right? Yeah.
DR. HOMER VENTERS: Some years, yes.
AMY GOODMAN: So, what is society’s responsibility here?
DR. HOMER VENTERS: I think that there are really very large policy decisions that have been made to keep these deaths and injuries hidden. And so, to undo these problems is not simply a matter of a little bit of training for one group of staff or another. It is that we have to establish medical systems that work not only to care for the patients and their health problems, but also to collect the data we do in the rest of the country, and report it out. We also need independent oversight. We’re fortunate in New York City to have the Board of Correction, an incredibly vital institution that really doesn’t exist in most of the other 3,000 counties in the States. But they need to be supported and the independence to make sure that the health service and the correctional service adhere to rules.
AMY GOODMAN: Dr. Venters, you also say Rikers should be closed.
DR. HOMER VENTERS: Absolutely.
AMY GOODMAN: Is it happening fast enough?
DR. HOMER VENTERS: Well, so, the Mayor’s Office of Criminal Justice, led by Liz Glazer, is doing an amazing amount of work to come up with the actual planning that can make it happen. But this is a political question. To close Rikers Island, one of the—
AMY GOODMAN: How many people does it imprison?
DR. HOMER VENTERS: The jail system today has about—has under 9,000. But we really need to get down to 5,000 or so, which means building at least another borough jail.
AMY GOODMAN: You write, the health risks that are faced, particularly by people with behavioral problems, in prison—talk about that.
DR. HOMER VENTERS: Yeah, I think that the most extreme example, that’s really an obscenity, is the notion that people who exhibit symptoms of mental health problems would be then put into solitary confinement, where we know that they’ll get worse and often die. And so, the idea that we had a solitary confinement unit for people with mental illness in the New York City jails until 2014 is horrific. It’s not—that’s not a lack of resources. That’s not a lack of thought. Thought went into it. And so, where Jason Echevarria and others died, you know, that was an affirmative decision. So, undoing those bad decisions, coming up with a more clinically appropriate, a therapeutic model, in most cases, means not having people in jail. It means having people in a community setting, that’s an actual healthcare setting. We built alternative models in the New York City jails, these units, the CAPS and PACE units, these very therapeutic units, but they’re incredibly expensive—couple million dollars a year for 20 patients. And every aspect of those units would be more effective if they were not in the jails.
AMY GOODMAN: Mass incarceration in this country has been taken on by grassroots activists now for years. And it’s certainly reading, I think, a—reaching a tipping point, where you have people across the political spectrum saying we have the largest prison population in the world. How can this be changed?
DR. HOMER VENTERS: I think that one of—there’s an important voice that needs to be brought to this, which is healthcare systems, health insurance companies, because keep in mind that while most people don’t die in jail or prison, many people are coming home with physical and psychological damage from these settings. And the care they need—which they may have struggle to access, but the care they need is going to be provided by community hospitals. Just take the example of traumatic brain injury. We documented all of the hidden traumatic brain injury just in the New York City jail systems. That increases the risk of those people for dementia and CTE down the road, that is incredibly costly to them and their families.
AMY GOODMAN: How do people on the outside get access to this information on the inside, particularly families of people who are in prison?
DR. HOMER VENTERS: So, I think that it is—these systems are designed to keep the truth from—certainly from families, who are, you know, lied to all the time. And from—but I think that it’s incredibly important to have aggressive journalism. But also, I think that some of the structures that exist in New York City should be replicated elsewhere, so having a board of correction or an oversight agency that demands data. Having investigative journalists that dig into individual deaths is incredibly important.
AMY GOODMAN: Steve Coll just wrote a new piece in The New Yorker, “The Jail Health-Care Crisis,” talking about the opioid epidemic, among other things.
DR. HOMER VENTERS: Yeah, I think that that’s a—that is also a very good example, that most jails and prisons, people don’t have access to evidence-based addiction care. So, many people end up incarcerated because of an addiction problem. Then, because they’re denied access to buprenorphine and methadone, they leave, and, we know—we have documented, here in New York City—their risk of death when they leave is much higher. Now, in New York City, we have a methadone program and a buprenorphine program for people who are incarcerated, but very few jails around the country have that.
AMY GOODMAN: And, Jennifer Gonnerman, what gives you the most hope as you continue to cover the prison-industrial complex?
JENNIFER GONNERMAN: Well, you know, as you were mentioning, there’s a lot of activists that have taken up this cause, which is fantastic, because, you know, back in the '90s, the 2000s, you just didn't see that level of interest or enthusiasm in activism for taking on these really challenging topics. That gives me hope. And also folks like Dr. Venters, people who have been on the inside, who have witnessed horrific things, and then have the wherewithal and the courage and take the time to really record them, so the rest of us can really, truly get a much better understanding of what’s going on behind bars.
AMY GOODMAN: And the access to information you, as a journalist, have, getting—for example, you leaked these videos of what was taking place with Kalief being beaten, the videos that are taken, the surveillance system within prison?
JENNIFER GONNERMAN: Right. You know, that was very unusual. You know, there is very little video footage that has come out of—from prisons around the country, despite there being a number of surveillance cameras. You know, like Dr. Venters said, the truth is hidden. It’s intentionally hidden. It’s very difficult—you know, reporting on what’s going on inside of jails and prisons is very difficult. But, obviously, the more journalists who are taking on the challenge, the more we’re going to get to the heart of what the truth is.
AMY GOODMAN: I want to thank you both for being with us. Dr. Homer Venters, former chief medical officer for New York City’s Correctional Health Services. His new book, Life and Death in Rikers Island. And Jennifer Gonnerman, staff writer for The New Yorker magazine. We’ll link to her piece, “Do Jails Kill People?”












Media Options