
Guests
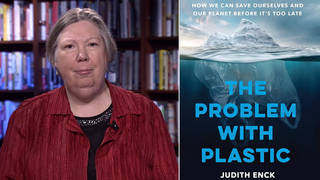
- Dr. Joia Crear-Perrypresident of the National Birth Equity Collaborative.
- Dr. Camara Phyllis Jonesfamily physician, epidemiologist and past president of the American Public Health Association. She teaches at the Rollins School of Public Health at Emory University and at the Morehouse School of Medicine.
When Black doctor Susan Moore died from COVID-19 after posting a video from her hospital bed describing racist treatment by medical staff, her chilling message was compared to the video of George Floyd begging for his life as he was killed by Minneapolis police. We speak to two leading Black women doctors fighting racial disparities in healthcare who wrote The Washington Post opinion piece, “Say her name: Dr. Susan Moore.” “It is a typical and ongoing devaluation of our lives and distrust of our word,” says Dr. Camara Phyllis Jones, a family physician and former president of the American Public Health Association. Dr. Joia Crear-Perry, president of the National Birth Equity Collaborative, says Dr. Moore’s complaints about being disrespected by medical staff are “really familiar” to her. “We’ve found that Black patients, Black birthing people are not valued; they’re not listened to,” she says.
Transcript
AMY GOODMAN: This is Democracy Now!, democracynow.org, The Quarantine Report. I’m Amy Goodman.
As we just reported, the death of a Black doctor from COVID-19 is shining stark new light on racism in medical care and how the virus is devastating Black communities. The Centers for Disease Control and Prevention reports Black and Latinx people are dying of COVID-19 at a rate almost three times that of white Americans.
Earlier this month, Dr. Susan Moore posted this now-viral video on Facebook describing racist treatment by medical staff who did not respond to her pleas for care, despite being in intense pain and being a doctor herself. She said in the video, “This is how Black people get killed.”
For more, we’re joined by two of the Black female physicians who wrote a Washington Post opinion piece headlined “Say her name: Dr. Susan Moore.” In it, they write, quote, “If anyone knew how to fight for herself, it would have been Moore. Still, she was sent home. Less than three weeks later, she was dead. … The deaths of [Mr.] George Floyd and so many others mistreated, injured or killed at the hands of our policing system have made us accustomed to seeing the video. But injustice in health care is rarely broadcast from cellphone videos or shared for thousands to witness,” they said.
Joining us in Atlanta is Dr. Camara Phyllis Jones, family physician, epidemiologist, past president of the American Public Health Association. She teaches at Emory Rollins School of Public Health and the Morehouse School of Medicine in Atlanta, Georgia. And in Washington, D.C., Dr. Joia Crear-Perry is with us, president of the National Birth Equity Collaborative.
We welcome you both to Democracy Now! Seeing that video that we just played of Dr. Susan Moore, she said, “I put forth, and I maintain: If I was white, I wouldn’t have to go through that.” Dr. Camara Phyllis Jones, if you would first talk about your response when you saw this heartbreaking, enraging video that Dr. Moore made from her hospital bed just before she died?
DR. CAMARA PHYLLIS JONES: Well, first of all, hearing it again is making me tense. She was fighting for her life. Many patients know that they’re not getting — they feel a little devalued. But she knew exactly what she should have gotten, and so she knew exactly how bad the treatment was. And so, here she was, calling out racism.
And the people there were intimidated, they said, in later statement, intimidated by her, intimidated by her asking to be valued for her own full humanity. Since when do we have to diminish ourselves and hope for scraps of care?
So I was angry then. I’m angry now. It’s another — just another naming of racism in this racist society. So, racism is not limited to healthcare. It’s not limited to policing. It’s in education. It’s in housing. It’s everywhere. It’s woven throughout the fabric of this nation. It’s foundational in our history.
AMY GOODMAN: Dr. Jones, Dr. Moore described how a white doctor questioned the veracity of her pain. Dr. Moore said the doctor, quote, “made me feel like I was a drug addict,” and, quote, “he did not even listen to my lungs. He didn’t touch me in any way.” Respond.
DR. CAMARA PHYLLIS JONES: So, that also is typical. We know, historically, there are these ideas of biological differences between the races, which do not exist. We have mapped the human genome. There is no basis in the human genome for biological subspecies. But people have — since Marion Sims experimented and perfected his surgical techniques on enslaved women without using anesthesia, up to the neglect of people with sickle cell anemia, when they come in with pain and are disbelieved or undertreated, or people with kidney stones, it is a typical and ongoing devaluation of our lives and distrust of our word.
AMY GOODMAN: So, let me bring Dr. Joia Crear-Perry into this conversation, president of the National Birth Equity Collaborative. Can you talk about both Dr. Moore saying that she felt like they were treating her as a drug addict instead of a doctor, even though they knew she was a fellow physician — and it shouldn’t take that — and what that means in your profession, and what you see, the fact that African Americans, like Dr. Moore, are dying at an astronomical rate of COVID-19? Already the country is in — across the country, people are dying, the worst record for deaths in the world, but the African American community is particularly hard hit.
DR. JOIA CREAR-PERRY: Yeah. Thank you so much.
Every time I hear the video, it saddens me again. It feels really familiar. The work that we do with the National Birth Equity Collaborative, working on Black maternal health, we found that Black patients, Black birthing people are not valued; they’re not listened to. So it felt very familiar, because I’ve heard it many, many times. If you see the stories over the last few years around the fact that we’re three to four times more likely to die in childbirth than our white counterparts — in places like New York City, eight to 10 times more likely to die — she is explaining to us how that happened.
When you come to a place and people do not evaluate you for your pain, they don’t believe you — you have to have a CAT scan to prove that you have pain? That doesn’t seem logical to most providers, that if you were to come in, that’s actually — we complain about expending too much money in healthcare. That was a wasted resource. You don’t need to get a CAT scan to prove pain. That’s not something that we normally do. We only do that to Black patients, to patients we don’t believe, to Brown patients, to Indigenous folks, when we say, “Well, you’ve got to prove pain, because you’re superhuman.”
That goes also back to what Dr. Jones was talking about, this legacy and this history of a belief in a biological basis of race. They’ve done studies to prove that medical students believe we have thicker skin — medical students. And I’m not saying that we’re picking on the medical students, because they’re being taught by deans and professors who are saying things like Black people have thicker skin. I mean, I was taught in my own medical school in the late 1990s, which is not that long ago, that there were three biological races: Mongoloid, Caucasoid and Negroid. So, that belief and that language that there’s a biological reason that we don’t feel pain and that we’re superhuman and that we’re —
And it’s also — it’s interesting to see that she was fighting for herself. She knew the right words. He even threatened her. You hear her. She said, “I’ll put you out at 10:00 at night.” We’ve seen those kind of things happen, where we tell patients, “If you don’t act right, I’m not going to give you this epidural.” Right? This threatening around “If you don’t behave the way I want you to behave, I will then punish you, because you’re asking to be valued and not to be in pain. You’re asking for things that are basic human needs, and therefore I don’t think you deserve those things, so let me punish you for even asking to be seen as human.”
AMY GOODMAN: So, in the piece that the four of you wrote, all African American women doctors, in The Washington Post, you compare the death of Dr. Susan Moore with the police killing of George Floyd. Dr. Joia Crear-Perry, you are not only a doctor in the hospitals of this country, but you were in the streets protesting George Floyd’s death. Can you talk about what you see is the connection?
DR. JOIA CREAR-PERRY: Well, there’s an overriding, -arching policing of Blackness. It was in law from the beginning. If you think about like after Reconstruction, we were — that people were told that they should make sure that Black folks don’t go into certain neighborhoods. They were not allowed, refused. To catch a slave running away.
You see these videos of even like recently: In New York City, a woman saw her phone was missing, and she assumed that a Black child had taken it, and went to attack the child, and felt that she had perfect permission as a white woman to attack a 14-year-old child, assuming that they had stolen her phone.
So, that belief that we’re supposed to be policed and organized and planned and controlled is embedded in policing and in healthcare. How we police women’s bodies — and it’s women plus being Black, both things, gendered racism, together — really gets the outcomes that we see, so that throughline.
I don’t want us to blame — and sometimes we’ll focus on the doctor who took care of Dr. Moore in Indiana. And yes, perhaps he should get some kind of accountability for his individual behavior. But the structure, the structural racism, is the undergirding of both our police system and our healthcare system, the belief in needing to control, the belief in needing to not value, to not listen to people, that we’re not having a co-created patient plan.
When we talk about patients, we say things like we want to have — co-create it, and we want to make sure that we have shared decision-making. If you don’t believe in the person that you’re sharing this decision-making with, if you think that they are not fully capable and not fully human, then there’s never really any shared decision-making. It’s authoritarian. And so, that’s the same thing that happens in policing.
So, if we are going to undo the racism that’s in this country, we have to start first with some truth, some historical truth about how we got here and some current truth about what happens today.
So, Dr. Susan Moore’s video gives us a — just the same way that George Floyd’s video did, we’re not just looking at numbers or data. We actually see the people who are being murdered, who are dying, hear their stories, see them as fully human and say, “Why would we ever do that to any human being ever? Don’t we want all people to have justice and joy? Don’t we want them all to be able to thrive?” We wanted George Floyd to still be here, and we also want Dr. Susan Moore to still be here. So how do we use their history and their legacy to build a better world for all of us?
AMY GOODMAN: On Tuesday, Vice President-elect Kamala Harris received a COVID-19 vaccination on live TV at the United Medical Center in Washington’s predominantly Black Anacostia neighborhood.
VICE PRESIDENT-ELECT KAMALA HARRIS: I have now been vaccinated. As Joe likes to say, there’s a big difference between the vaccine and vaccinations. I want to encourage everyone to get the vaccine. It is relatively painless. It happens really quickly. It is safe, the Moderna, the Pfizer. Today, I had the Moderna vaccine. My husband is going to have it today, as well. I look forward to getting the second vaccine.
And literally, this is about saving lives. It’s literally about saving lives. I trust the scientists. And it is the scientists who created and approved this vaccine. So I urge everyone: When it is your turn, get vaccinated.
AMY GOODMAN: So, of course, the vice president-elect, Kamala Harris, will be the first African American and African American woman vice president in U.S. history. And she was injected by Patricia Cummings. She was vaccinated by this African American nurse, who is the daughter of Guyanese immigrants.
The significance, Dr. Camara Phyllis Jones, of seeing this image clearly in the Black community of Washington, D.C., being vaccinated by a Black woman, the Black woman vice president to be? The message that is being sent, as African Americans, studies show, are — perhaps 40% are now willing to get a vaccine? What do you think needs to be overcome for the Black community to feel more comfortable with this vaccine, given the history, you said, for example, of Marion Sims, considered the father of modern gynecology, experimenting on enslaved women?
DR. CAMARA PHYLLIS JONES: The first thing is that we don’t need to go out trying to convince people to get the vaccine. We need to honor and hear their questions, answer their questions. And in some cases, the answer to the question could be “I don’t know,” because there is a lot that we still don’t know about the long-term effects of the vaccine or the rare effects.
But I do have to say that when you look at the benefits and the risks, I have decided that when my turn in line comes, I will get the vaccine, because even though there is uncertainty — there are things that we don’t know, because the virus is new and the vaccine is newer. You know, we haven’t been studying it long, and we haven’t studied it in a whole lot of people. But we live with uncertainty in our lives. I am willing to live with the uncertainty associated with the vaccine, as opposed to dying with COVID-19, which is a much bigger risk. The whole issue is a risk-benefit analysis. Both the Pfizer and Moderna vaccines have shown themselves to be highly, highly effective.
So, what we need to do is not try to say, “Oh, those people, why don’t they just get over that history?” or, “Oh, those people, why do they have all these questions or this distrust?” First of all, we need to make sure that we evidence trustworthiness in all of our systems, going forward. Dr. Susan Moore’s example was not an example that engenders a feeling of, you know, trust, because the system was not trustworthy in her case. So, all of our systems, if we want to convince people to get the vaccine, have to evidence themselves to be trustworthy.
And we, as a nation, need to say, “We honor your lives, not just when you get the vaccine, but we honor your lives, and we’re going to provide the support you need to safely shelter in place. We are going to provide the regulations that the workplaces need, that if you have to go to work, they are safe workplaces. We’re going to provide you with the PPE that you need as a grocery clerk or as a bus driver or a warehouse worker to keep you safe.” It’s not just, “Oh, now that we have the vaccine, we want to convince you to take the vaccine, because, well, maybe we’re worried about herd immunity, and we’re really not worried about you at all, but, you know, to get to herd immunity, we need to do this.”
No, be trustworthy in all ways, and be about my people, my community, my health in all ways. That’s the evidence that is going to really convince people that, yes, maybe I should take the vaccine.
But I have to say, at the individual level right now, risk-benefit, I agree. I can live with the uncertainty, because these two vaccines, in particular, have shown themselves to be highly efficacious.
AMY GOODMAN: I want to put this question to Dr. Joia Crear-Perry. In 2018, tennis star Serena Williams and her husband, the Reddit co-founder, Alexis Ohanian, welcomed into the world their daughter, Alexis Olympia Ohanian Jr. The baby was born by an emergency C-section. Williams told Vogue magazine how she self-diagnosed a life-threatening emergency after giving birth. Shortly after delivering, the tennis star suddenly felt out of breath and assumed she was having a pulmonary embolism, given her history of blood clots.
I want to read from the 2018 piece in Vogue by Rob Haskell that describes Serena Williams’s birth experience: quote, “She walked out of the hospital room so her mother wouldn’t worry and told the nearest nurse, between gasps, that she needed a CT scan with contrast and IV heparin (a blood thinner) right away. The nurse thought her pain medicine might be making her confused. But Serena insisted, and soon enough a doctor was performing an ultrasound of her legs. 'I was like, a Doppler? I told you, I need a CT scan and a heparin drip,' she remembers telling the team. The ultrasound revealed nothing, so they sent her for the CT, and sure enough, several small blood clots had settled in her lungs. Minutes later she was on the drip. 'I was like, listen to Dr. Williams!'”
So, Dr. Joia Crear-Perry, you are president of the National Birth Equity Collaborative. Talk about the significance of what Serena Williams brought to life when it comes to postpartum deaths of African American women.
DR. JOIA CREAR-PERRY: Thank you. You know, I also want to show the throughline between Dr. Susan Moore and Serena Williams. Both of them are experts on their body, and they were seen as not experts, right? They both said, “This is what’s happening. This is what I need.” And the more that they could articulate expertise, the more that the people around them didn’t know what to do with them, because they were so accustomed to the bias inside of them saying, “These people aren’t experts. They don’t know what they’re talking about. I know better. I am the one that’s in control.” And that is the tension that we see when it comes to racism as a structure. I don’t want us to, once again, focus on individuals, but really the structures of how this plays out.
So, for us, we knew, when we found out, about six years ago, through Amnesty International, and the U.N. had sanctioned the United States around the fact that we had the worst outcomes for birthing people in the world, and then that Black people were three to four times more likely to die within a year of childbirth than their white counterparts, that we saw that — we knew that the language was going to be: “Of course they die. They are so fat. They don’t listen. They don’t go to the doctor.” All the blaming and shaming that normally happens to communities of color, the same thing that happened during COVID-19: “Of course they’re dying. They have all these preexisting illnesses. Of course. They all live together, and they don’t follow instruction.” Meanwhile, we’re more likely to put a mask on than anybody else. We’re more likely — we clean not only other people’s houses, we clean our own houses, so we’re usually extra sanitary, because we’re cleaning up for you and for ourselves. So this idea of blaming and shaming, we knew that was going to be the language.
So, Serena Williams was so important, because it showed that a person with wealth, with stature, with grace was, once again, not believed, seen as a poor historian of her own health, even though, if anybody, she’s paid her entire life, since she was a child, around her health. She knows her body better than anybody, because she’s a professional athlete. Professional athletes know everything about their bodies, because that’s how they make money. That’s how they live. For them not to listen to Serena, man, what does that mean for people like Susan Moore or like me or like any of us?
From birthing to elder care, it’s the same throughline of disbelief, of not having trust. When you talk to patients — our work, when we talk to patients that works with hospital systems, from big ones like Kaiser to little ones in Kalamazoo, Michigan, every one of them, what the patients want, when we talk to patients, is to be trusted. They want you to think and know that no matter their skin color, no matter their gender, no matter where they live, that they want justice and joy, that they want — that they are good historians. You don’t write things down like “noncompliant.” When you’re doing those things, you’re blaming and shaming the patient and really not thinking about all the things that could be happening.
So, Serena coming forth and talking about her — she also reminded me so much around how she walked outside because she didn’t want to scare her family members. That’s typical Black woman, right? Like, “I don’t anybody to get upset, so let me just go out here and just mention right quick that I might be dying, and this is what I need.” And then, she knew exactly, the same way that Dr. Susan Moore did: “These are the medicines that I need. This is the testing that I need.”
And unfortunately, when we show expertise as Black people, because we have not been historically seen as experts about anything, well, people don’t know what to do with that. So, nurses, doctors, systems, cultures, when we show up as the expert, we can feel the nervousness that others have around our expertise. But we’re like, “That’s your bias, not ours. That’s your assumptions about who I’m supposed to be, the box you’ve put me into.”
And wouldn’t it be amazing for all of us to let go of all of those boxes, to see Serena, Dr. Moore, to see our patients who live in Bogalusa, Louisiana, anywhere, as experts on their own bodies, that they have value, that they have thoughts and ideas that are amazing, no matter where you live, no matter your race or your gender?
And that’s really what we’ve learned through the Black maternal health work, working inside of hospitals, that when you look at your data, when you disaggregate your data, without question, Black patients will receive pain management later, they get their hypertension treated later. And you can really undo that. You can stop the structure of the system and say, “We are devaluing people, and we’re not going to do that anymore. We’re going to really see all of them and believe them and trust them and invest in them and make sure that they all can be seen in the future.”
AMY GOODMAN: Talking about throughlines, as we wrap up, Dr. Joia Crear-Perry, I think of Erica Garner, who was a guest on our show a number of times, fierce fighter against police brutality. Erica was the daughter, of course, of Eric Garner, who was killed by police in Staten Island. Erica would die just after giving birth to her second child, when she was just 27 years old. We did a show on Erica and Serena Williams showing that throughline. As we wrap up, a final thought on the Lancet study that you did, the respected international medical journal, called “Moving towards anti-racist praxis in medicine”?
DR. JOIA CREAR-PERRY: Yeah, and I just want to highlight that throughline. She died from cardiomyopathy. Her heart was enlarged. Just think about that. The stress of trying to fight for the value of her father and for his death not to be ignored and to hold the policemen accountable, ultimately, caused her heart to weaken — the stress of having to fight for humanity. For years, we liked to blame genetics on cardiomyopathy and looking for what the gene is that makes people’s heart weaker. But we know that your stress, your mental health, impacts your physical health. And until we undo racism, we’re going to see Black folks having higher rates of obesity, higher rates of hypertension and higher rates of cardiomyopathy. And that throughline of racism is consistent for all of us. And that’s what’s shortening all of our lives. So we need that to end.
And that’s what we talk about in this antiracism praxis. If I was taught in medical school, as I was — I was taught that there were three biological races — that’s racism. Racism was not created by God. Racism was not created by medicine. Those things have been — racism was created by people who wanted to hold power and wealth. And so, our job is to fight for equality and justice and joy, and to say, “How do we undo all these places inside of medicine where we say that Black people have different lungs or different kidney capacity or different pelvis shapes?” All this talk that we have a different shape of our pelvis, how could that possibly be, when it’s just melanin production that makes us different? That’s the only one difference. Our pelvis and our melanin have nothing to do with each other. So, really undoing those racist ideas that we were all taught inside of medicine —
AMY GOODMAN: Well —
DR. JOIA CREAR-PERRY: — so that we can have antiracism. Sorry.
AMY GOODMAN: I want to thank you so much for being with us, Dr. Joia Crear-Perry, president of the National Birth Equity Collaborative, and Dr. Camara Phyllis Jones, family physician, epidemiologist, past president of the American Public Health Association, teaching at both Emory School of Public Health, as well as the Morehouse School of Medicine. We will link to the piece they co-authored with two other African American women doctors in The Washington Post, “Say her name: Dr. Susan Moore.”
When we come back, “The truth in Black and white: An apology from The Kansas City Star.” Stay with us.










Media Options