
Topics
Guests
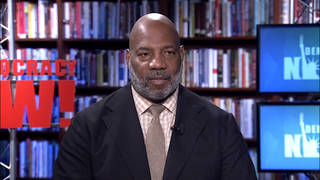
- Cleavon Gilmanemergency medicine physician in Yuma, Arizona, and Iraq War veteran who served as a Marine combat medic.
As the U.S. averages more than 200,000 new COVID-19 cases per day, we speak with Dr. Cleavon Gilman, an emergency physician who has been treating patients since the beginning of the U.S. outbreak, first in New York City and now in Yuma, Arizona. Dr. Gilman is also an Iraq War veteran who served as a Marine combat medic, and has kept a public diary of his experiences treating COVID-19 patients. He was fired after tweeting that Arizona’s ICU beds were full, and then got his job back after public outcry. “This pandemic is worse than being in Iraq,” says Dr. Gilman. “This virus is a Trojan horse, and it just hides in people, and you can bring it home to your family and infect every person in your house.”
Transcript
AMY GOODMAN: The United States hit the grim milestone of the worst day yet of the coronavirus pandemic this week, with 3,350 COVID-related deaths Tuesday alone. This comes amidst reports that 2020 has been the deadliest year in U.S. history. The United States is on track to top 3.2 million deaths this year, with 400,000 more deaths than in 2019.
As the country averages more than 200,000 new COVID-19 cases per day, we go now to the frontlines of the crisis to speak with a doctor who’s been treating patients since the beginning of the U.S. outbreak, first here in New York City and now in Yuma, Arizona, a COVID hot spot with nearly four times more cases per capita than the rest of the country. Yuma is home to one of the world’s largest military installations, also a massive prison facility where more than 600 prisoners recently tested positive for COVID-19 and the prison warden died after COVID complications.
Dr. Cleavon Gilman is an emergency medicine physician who received the Moderna vaccine on Thursday [sic]. He’s also an Iraq War veteran who served as a combat medic and deployed with the Marines in Iraq’s Al Anbar province, but he says that experience did not prepare him for the coronavirus.
Dr. Gilman has been keeping a daily public diary of his experiences treating COVID-19 patients. He says he was fired by Yuma Regional Medical Center after he sent out a tweet saying, simply, quote, “no more ICU beds in the state of Arizona.” But after public outcry, he was given his job back. He’s joining us now from Yuma, Arizona.
Dr. Gilman, you tweeted some pictures from two years ago, when you chaperoned a class trip of fourth graders to our Democracy Now! studios. It’s great to have you back as a guest, so unfortunate under these circumstances. Just a little correction: I know you got your vaccine yesterday. How are you feeling? And then talk about what’s happening right now in Yuma, why you risked your job — actually, lost your job — talking about the conditions in the hospital, and then got it back, because the community said, “No, you were a vital resource in Yuma.”
DR. CLEAVON GILMAN: Yeah. Thank you for having me, Amy and Juan. I’ve been a big fan of this show for actually years, so it’s a real honor to be on here.
Yeah, I got my vaccine yesterday, the Moderna vaccine. And it was a bit — you know, I was a bit uneasy about it, because there have been 310,000 people who have died from the virus. I’ve lost three of my colleagues, as well: Romy, Mary and Lorna Breen, who took her own life. I’ve also had a 27-year-old cousin, as well, who has died from the virus. So, you know, of course, getting this vaccine was a bit of survivor’s guilt, in a sense, I feel. But I’m feeling great. I have a bit of a soreness in the arm now, but otherwise I feel great.
The condition here in Yuma, Arizona — it’s crazy, because I was in Manhattan, and then I fly out here, I move my whole family out here, and this is a hot spot, as well, too. But it’s the same deadly pandemic here as it is in Manhattan. I think the only thing that’s kind of changed is the volume of patients. There’s not as many patients here in Yuma, Arizona. However, the resources are not the same here, as well, too. We have less staff here. It’s the only hospital for hundreds of miles, and so our hospital is seeing an unprecedented number of patients who have COVID.
The tweet that got me so — I guess I’ll just begin with saying that I have a moral obligation to telling people the truth about this pandemic. I’ve seen countless people die in New York. And since March, I’ve been keeping a journal about that. And so, here, the week prior to November the 20th, I was seeing more and more patients who had COVID. And so, our governor here, Governor Doug Ducey, was telling everyone that there were 180 ICU beds. So, then I showed to my shift, and I’m unable to transfer three ICU patients. And I had to manage those patients in the ER and see brand-new patients at the same time. So I put out a tweet. It went viral.
The next day, I was advised I was not able to return back to the job. My medical group tried to negotiate over the next three weeks, and the hospital refused to let me return, despite four doctors being out with COVID, as well. And so, eventually, I talked to a reporter, and she dropped an article, and then there was a huge public outcry to have me return back to work.
JUAN GONZÁLEZ: Well, Dr. Gilman, as Amy mentioned earlier, Yuma is also home to a massive military base and prison complex. Can you talk about how these types of facilities have contributed to the spread of COVID-19, from what you’ve been able to tell?
DR. CLEAVON GILMAN: Yeah. It seems the first case here actually came from a soldier on the base, so that’s how it was introduced to the community here. So, there are a lot of military personnel and a lot of retired personnel, as well, here.
I’m seeing a majority of the cases here, though, are not from the military, though. They’re from underserved populations here. Sixty percent of the people here are Latino, so I’m seeing a large majority of those patients who have the virus.
And the prison here, there’s a huge prison outbreak here: 650 people who have the virus. And those patients are beginning to trickle in to the ER. Sadly and tragically, the prison warden even died from the virus, we think.
JUAN GONZÁLEZ: And what about the virus’s impact on the Navajo Nation in Arizona?
DR. CLEAVON GILMAN: So, the Navajo Nation was having a lot of problems in June, I believe. Since then, however, they have managed strict lockdowns and were actually controlling the virus pretty well, until about three weeks ago. They began having increased cases again. I’m not seeing a lot of Navajo Nation patients in the place I’m at, though, particularly.
AMY GOODMAN: Dr. Gilman, your life story is really astounding. I mean, you quit high school maybe because you were being bullied for your stutter, and it was too humiliating for you. You end up in the military. You start to deal with bodies in Iraq. Tell us this story, where you end up being — coming back to this country and going to some of the most elite institutions and becoming an emergency room doctor. Talk about your time in Iraq and how this compares to Yuma.
DR. CLEAVON GILMAN: Yeah, I just remember — so, when I grew up, I wasn’t really supposed to be anything in life, honestly. I would go on job interviews. I would be this discriminated against because of how I dressed and my speech impediment, as well, too. So I joined the military, and I had an opportunity.
But being in Iraq, I was 24 years old, and I remember flying in to Iraq. And everyone just — they don’t teach you about the enemy, right? They dehumanize the enemy there. So everyone was like — we were kind of flying in, and everyone was like, “I can’t wait to kill an Iraqi. I can’t wait to kill this person.” And, you know, there’s a lot of hate and a lot of a kind of group anger towards the Iraqi population. And so I get there, and the first day I’m out there, a soldier kills himself out in Kuwait. And then we get mortared, and I start treating casualties out there, and I start putting 18-year-olds in body bags. And that changes you as a human being.
I also worked at a prison out there, too. And I got to see this person I was kind of trained to hate. And I was like, “This person does not look very evil to me.”
So, I come home. I get out of Camp Pendleton. I get out in California, and I begin this journey at the community college, Southwestern Community College. And I just stay on the campus for 12 hours a day, and I just hit the books every day. And then I’m able to transfer to UC Berkeley, where I’m learning about the war, as well, like the Iran-Iraq War, and exactly how these people were killing us with our own munitions.
But this pandemic is worse than being in Iraq. And I say that for a lot of reasons. You know, there are some similarities between it, right? You have on a mask. You go in a uniform to your job. You have this camaraderie with your people on the frontlines. You have nightmares of the patients you treat.
But this virus is a Trojan horse, and it just hides in people, and you can bring it home to your family and infect every person in your house. It’s also an invisible enemy; you can’t see this virus, as well. And this battlefield is — we are going into war through the hospitals, and we’re treating patients, and then we’re driving home past a crowded gym, past people eating, and they’re totally oblivious to the people that are dying here in Arizona, in New York, as well. And there’s also just an unprecedented amount of death here. There’s 3,000 people who are dying a day.
We also don’t have any support from the president at all. I mean, he even accused us of like — he accused us of falsifying COVID deaths. He accused nurses of taking PPE. He contributes to the actual patients with these maskless rallies, as well.
And the other thing is, you can’t escape this virus. It’s everywhere. You know, I can’t just, like, fly out of Iraq and be safe. It’s everywhere. So, it’s a lot harder. You know, it truly is. And, you know, this —
JUAN GONZÁLEZ: Well, Doctor, I wanted to ask you — in terms of that, you mentioned earlier that one of your colleagues committed suicide. I’m wondering if you could talk a little bit about the emotional toll this has taken on health workers, like yourself, dealing with this pandemic.
DR. CLEAVON GILMAN: Yeah, yeah. You know, I trained for war, and so I’m a bit more equipped than my healthcare providers out there. But it’s not normal. It’s not normal to see this many people dying per day, gasping for breath. And I want to be very clear what these patients are looking like. Imagine running on a treadmill full speed and hopping off of it and gasping for breath. That’s how these patients are coming into the ER. And they’re crashing very quickly. I just intubated a teen the other day, you know, and they say young people are not affected by this virus.
And one of the hard parts of this, opposed to being in Iraq, is, in Iraq, I didn’t have to sit across from a loved one in a consultation room and tell them that their son, their husband or wife has died. And that, it’s there in the brain. It rises up at times, and it’s really hard to do this job. And that’s how come, like, a lot of us, we need your support, as well, too. I had a colleague, Lorna Breen, that took her own life. And it’s just really hard for us. I’ve had colleagues who have been intubated. We are under a lot of strain, and we are not getting any support. I would appreciate it if people would support the Lorna Breen Act, which will provide grants for mental health programs for healthcare workers.
AMY GOODMAN: Dr. Gilman, you worked with Dr. Lorna Breen. She was head of the emergency room at NewYork-Presbyterian. So you’ve been at two epicenters of the pandemic, in Yuma now and, before that, here in New York when it was at its height. Stat News did a profile of you, one of the most respected health websites. And they show a picture of you in a hallway of NewYork-Presbyterian here in New York, where you’re sitting by yourself in what you call “the bad news chair,” because you used it when you phoned families of patients who had died, the idea that you’re not only desperately trying to save lives, but you’re often, along with nurses and other hospital staff, the only people around a patient when they die. Talk about that chair.
DR. CLEAVON GILMAN: My god, Amy. The chaos in the emergency room in New York is unlike anything I’ve ever experienced before. We were intubating, putting breathing tubes in 20 to 30 patients per day. And I was calling two to three loved ones in a day to tell them that their family member died.
And let me tell you about the job that I — you know, it’s really hard to be an ER doctor. It’s really hard to be an ER nurse. And it’s hard when you see your community that is being killed by this virus — janitors, grocery workers, bakers, everyone in — you know, like, my whole community was dying from this virus. And so, I would have to call, and I had to have a place that was very quiet. And so I would kind of prepare myself for that moment.
And it’s always the same thing. I would call up, and they knew I was going to give them very bad news. And it’s just, honestly, like — it’s just this shrill cry that they say. And even worse when the person on the phone had to translate it, and you heard it twice, and it’s just a dagger in the heart over and over again, and, you know, just countless times throughout my shift throughout the pandemic. And it’s really hard on us. We are going to have a lot of PTSD in this country. And it’s just horrible. It’s a horrible disease.
JUAN GONZÁLEZ: Dr. Gilman, you recently had the chance to speak by phone with President-elect Joe Biden. What is your hope that the incoming administration will do differently from what has been coming from Washington so far?
DR. CLEAVON GILMAN: Juan, Juan, Juan, come on, yo. Joe Biden is an ally. He’s not going to, like, downplay the virus and create more and more kind of patients. I talked to President-elect Joe Biden. It was great. He is an ally. He’s going to mandate masks. He is going to use the Defense Production Act to actually increase the amount of N95 masks, so that hopefully everyone is able to have one. He’s going to actually do something called contact tracing, which we have not done in this whole country at all. And then also just speak the truth, right? Put people who are experts to talk about the virus — right? — you know, to tell people, “This is a deadly virus. Here’s what you need to do. You need to wear a mask. You need to socially distance. You need to avoid indoors.” So, I am very hopeful.
But the problem is — right? — this virus is out there. There’s over 200,000 to 300,000 new infections per day. Up to 3,000 people are dying. He’ll be in there on January 20th; however, 'til then, there's a long period where people are going to die, as well, and the virus is going to be spreading.
AMY GOODMAN: Final words for Governor Ducey and President Trump, even as President Trump will be leaving soon, whether he is accepting this or not? There are so many days between now and January 20th, days where thousands of people will die. What do they need to do? You in a state where there is no national mask mandate, as there aren’t in most states.
DR. CLEAVON GILMAN: Yeah. Governor —
AMY GOODMAN: Or state ones.
DR. CLEAVON GILMAN: Our hospitals are at capacity right now. It’s kind of unchanged since the 23rd. We need hard-line measures. We need a statewide mask mandate. We need to close the bars. We need to close the schools. We need to control this virus. And we need top-down leadership, not for him to punt the responsibilities to local mayors, who feel the brunt of that, of making the orders.
AMY GOODMAN: Well, Dr. Cleavon Gilman, it’s been a pleasure talking to you, emergency medicine physician in Yuma, Arizona, also treated COVID-19 patients here in New York City at the epicenter of the pandemic here, an Iraq War veteran who served as a Marine combat medic.
When we come back, we look at Joe Biden’s pick for secretary of education, Miguel Cardona, former elementary school teacher who now oversees schools in Connecticut. By the way, our music break is by our guest, Dr. Cleavon Gilman, who says, when he raps and sings, the stutter just goes away. It’s “Rise Up Now.”
[break]
AMY GOODMAN: That’s Dr. Cleavon Gilman singing “Rise Up Now.”










Media Options