
Guests
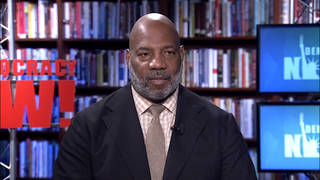
- Dr. Craig Spencerdirector of global health in emergency medicine at Columbia University Medical Center. Dr. Spencer, who contracted Ebola while fighting its outbreak in Africa, is now an emergency room doctor in New York City, where he is treating coronavirus patients.
As New York hospitals see a surge in coronavirus cases, medical workers report growing shortages of protective gear, and a nurse who tested positive after treating patients with the highly contagious disease has died. “It’s pretty dire inside New York City hospitals right now,” says New York City emergency room doctor Craig Spencer. “We have a growing number of patients coming in every day with coronavirus. We have people young and old, with complications, without complications, who get put on mechanical ventilators, who get put on life support to help their breathing, who have cardiac arrest. It’s a daily reality for many of my colleagues on the frontline.” Spencer is also a survivor of Ebola, which he contracted while fighting its outbreak in Africa.
Transcript
AMY GOODMAN: We’re going to begin right here in New York City, the epicenter of the coronavirus outbreak in the United States, hospitals seeing the same surge in coronavirus cases that overwhelmed healthcare systems in China, Italy and Spain. Refrigerated trucks and tents have been stationed outside of some hospitals to hold the bodies of the dead as morgues fill up. In 24 hours on Tuesday, 13 people reportedly died at Elmhurst Hospital Center, a 545-bed public hospital in the borough of Queens. The New York Times reports, quote, “In several hours on Tuesday, Dr. Ashley Bray performed chest compressions at Elmhurst Hospital Center on a woman in her 80s, a man in his 60s and a 38-year-old who reminded the doctor of her fiancé. All had tested positive for the coronavirus and had gone into cardiac arrest. All eventually died.” Dr. Bray called the situation “apocalyptic.”
New York City is reporting 366 deaths and more than 33,000 confirmed cases — almost half of all the cases in the United States, though the number is expected to be so much higher due to the lack of tests. More than 4,000 coronavirus patients have been hospitalized in New York City. A leaked FEMA briefing shows all the more than 1,800 intensive care beds in the city are expected to be full by Friday, and the state has called for tens of thousands more ventilators, hospital beds and intensive care beds.
This comes as workers at New York City hospitals report shortages of personal protective equipment as they work amidst patients with the highly contagious disease. Workers for the massive Mount Sinai Health System shared photos online of themselves wearing trash bags for protection. A New York City nurse who was treating coronavirus patients has died after testing positive about two weeks ago. Mount Sinai West nursing manager Kious Jordan Kelly was in his forties, and his co-workers described him as compassionate, devoted to his patients.
For more, we’re joined by Dr. Craig Spencer. He is director of global health in emergency medicine at Columbia University Medical Center. Dr. Spencer contracted Ebola while fighting its outbreak in Africa and survived the disease. He’s now an emergency room doctor in New York City, where he’s treating coronavirus patients. He’s also on the board of Doctors Without Borders. And again, with us, our co-host Nermeen Shaikh.
We welcome you both to Democracy Now! Dr. Craig Spencer, describe a day in the New York City hospitals. We just laid out this graphic picture of shortage. And the question is: How unnecessary was this, the idea that in this country, the richest in the world, doctors, people like you, and nurses and the staff of the hospitals, going to those who even clean the hospitals, do not have access to the necessary protection to treat the patients that are surging into these hospitals?
DR. CRAIG SPENCER: Thanks for having me on, and let me share the story. Look, it’s pretty dire inside New York City hospitals right now, and we’re all concerned about how that’s going to spread throughout the rest of the country, or, more frankly, the rest of the world. It’s no surprise that the greatest number of cases are being reported in the places with the strongest or the best healthcare systems. We know that cases are spreading all over the world. We’re just picking them up more here, and we’re seeing a lot more of the complications inside of our emergency departments. As has already been reported, we have a growing number of patients coming in every day with coronavirus. We have people young and old, with complications, without complications, who get put on mechanical ventilators, who get put on life support to help their breathing, who have cardiac arrest. It’s a daily reality for many of my colleagues on the frontline, especially here in New York City.
AMY GOODMAN: Nermeen?
NERMEEN SHAIKH: I’d like to ask you, Dr. Spencer — I mean, one of the things, as Amy mentioned, that’s very striking is that the U.S. is, of course, extremely wealthy, the wealthiest country in the world, but it also has — according to the Global Health Security Index, in 2019, the U.S. was the highest-ranked country in terms of pandemic preparedness. The U.S. was the best prepared. So, if American hospitals are being overwhelmed in this way, what about all of the other countries that don’t have the resources that the U.S. does?
DR. CRAIG SPENCER: Yeah. I think if you asked anyone over the past couple years whether — anyone that does this for a living, whether or not the U.S. was prepared for a pandemic, we all would have said no. I think all of us have written articles in the past couple years lamenting the fact that the U.S. has torn apart the preparedness architecture here in the U.S. by underfunding the CDC, by underfunding state and local departments of health. It’s not surprising to anyone that’s been looking at this or been worrying about this over the past couple years that this pandemic is wreaking such havoc here in the U.S.
We’ve also drastically underfunded the World Health Organization, despite the lessons we learned in West Africa in 2014 to 2016 with the Ebola crisis there. We learned that having preparedness was much more important than a reactive response. We learned that putting the right amount of funding into the organizations who are capable of picking up these disease threats and responding to them all over the world is the only way to protect people everywhere. It is so much cheaper. It is so much cheaper to invest in preparedness than it is to scramble for response. We’re putting together trillions of dollars to try and respond to this just here in the United States. And that amount of money would have provided for global preparedness for over a decade.
And so, we need to really think about our priorities. And I hope when we come out on the other side of this, we think about where the smart investment is. The smart investment is not just trying to build a wall around this country with the hope that we’re going to keep microbes and bacteria out. The reality of our world right now is that wherever a disease starts — and it’s more likely to be in China than it is to be in Columbia, Missouri — it can be anywhere in the world within 24 to 48 hours. And we are all at risk, unless we have strong health systems in the places where the most vulnerable patients are.
NERMEEN SHAIKH: And, Dr. Spencer, can you explain, for people who don’t know, the people — I mean, in the U.S., most healthcare is privatized. So, why is it that in private hospitals there is not sufficient — there isn’t sufficient personal protective equipment? Because not funding the CDC or cutting funding to the CDC, etc., shouldn’t impact the decisions that private hospitals make about the equipment, the beds, etc., that they acquire.
DR. CRAIG SPENCER: Yeah. You know, it’s funny, because we talk about these N95 masks. Those are those thicker variants that filter particles like the coronavirus. And generally, we’re fit-tested in the hospital every year — it’s a requirement — to make sure that they fit right, that nothing can get through. We almost never use them, because in the U.S. we don’t have relatively many tuberculosis patients. We don’t have a lot of people where we have to use this type of protection. That’s not the reality in many of the places that I work — West Africa, East Africa, Southeast Asia, etc. There, they are just more used for a lot of the communicable diseases that we have stopped seeing as much here in the United States.
The result is that a lot of my colleagues don’t have the same amount of experience of working with the personal protective equipment that we need right now. I see a lot of people who are, you know, touching the mask or putting it on or taking it off incorrectly. Personal protective equipment like gloves and masks do not protect you if they’re used incorrectly. One of the greatest risks when you’re using them is taking them off wrong, touching your face, touching the mask and infecting yourself.
So, it’s not surprising that we don’t have a huge supply of these things. We didn’t prepare for this scenario. And I think this is the most important message. So many people knew that this was coming. So many people knew that this was coming. You can look back, and you can see headlines from three month ago, three years ago. Everything that we learned in West Africa seemed to have been torn apart in decisions that, you know, seemingly undermine our willingness and our ability to respond to pandemics, not only here in the United States, but throughout the world.
AMY GOODMAN: Dr. Spencer, if you would take us on your personal journey, what happened to you when you were dealing with Ebola in Africa, about contracting it, and then the lessons we can learn? And I want to particularly go to the issue of the egregious lack of tests and how that is a major public healthcare measure, just for people to understand, the lack of tests, the lag in getting them, and then even now the amount of time it takes for people — it can be four, five, 10 days to find out, in fact, even if they get the test — in New York, very difficult — and what that means in terms of contagion. But start with yourself contracting Ebola.
DR. CRAIG SPENCER: Yeah. So, I worked in West Africa, in Guinea, in 2014. I was in Guéckédou, another epicenter of an outbreak, providing direct clinical care on a daily basis, in full protective personal equipment, with Doctors Without Borders. And I followed rigorous protocols every single day. My organization had been doing this for decades and had really done a great job in minimizing the risk to the providers and increasing the quality of care we could provide to our patients.
That being said, personal protective equipment is not flawless, it’s not perfect, even if used perfectly. At one point I was infected. When I came back to the U.S., I was, thankfully, treated here and received incredible quality care and was lucky enough to survive, largely because I was treated in a really great health system. I was also really young and didn’t have any other medical issues. But the whole time, the only thing I could think about were my colleagues and my friends back in West Africa that didn’t have access to the same quality of care. One thing I say is that in West Africa I took care of about 30 patients myself at any time, and here in the U.S. I probably had 30 providers on call to take care of me at any time.
Some of the stunning similarities and differences between West Africa and coronavirus is that, yeah, they’re both viruses. The coronavirus seems to infect more people and kill a relatively smaller percent versus Ebola. But the difference in terms of the fight was that in West Africa, I at least never really had to worry about my personal protective equipment. A lot of my colleagues here in New York City are worried about the number of N95 respirators we have, how limited our supply chain is. And if it’s bad here, what is it going to look like in the rest of the country?
And you bring up another really important point that we haven’t talked about, I think, enough, and that is this issue of testing. Right now we’re talking about only testing certain people, so only testing some healthcare workers, only testing people that are hospitalized. It’s not because that’s the best thing to do. It’s because that’s really the only thing we can do right now. Testing capacity has increased dramatically in the past couple weeks, but we are months delayed. We should have had a testing strategy like South Korea. We need to understand where this disease is, is passing, where it’s transmitting. And the only way to do that is to test, test, test and test. We haven’t been doing that. We’ve all been limited in our hospitals and in our communities. People are walking around now not knowing whether or not they’ve had coronavirus, whether they may have some type of immunity, whether they could be out in our communities helping other people, if they have antibodies, by delivering groceries to the elderly or helping in other institutions. So, our testing strategy right now is such because we failed to be prepared. There were critical missteps in the testing capacity, in the testing kits that were sent out. There were a lot of promises about our ability to do billions of — millions of beautiful tests for anyone that wanted one. That was never the reality on the frontline, and that’s completely changed in the past couple weeks.
AMY GOODMAN: So, Dr. Craig Spencer, if you could talk about the use of it as a public health measure, that you understand, and now, as a result, everyone must treat themselves as if they are contagious, as if they’re infected, to protect others in the community, and yet you have President Trump — if you can respond to what he is saying, that by Easter — right? — in just a few weeks, he wants to see packed churches, while the pope at the Vatican is telling people to wash their hands but not wash the feet of the worshipers, while he is saying pray at home? Of course, he’s in Italy, which is so hard hit. And many are deeply concerned that the U.S. could go that route. What would stop us from going that route? And talk about the danger of President Trump’s message.
DR. CRAIG SPENCER: Yeah. I think, in a week, we will be Italy. At least here in New York City, we’re already seeing that. This is something I’ve been warning about for weeks. This is something Italy has been warning us about for weeks. In terms of what can stop this, I don’t want to incite any panic; I want to incite some kind of preparation, because we still have a huge country outside of New York City and the other epicenters right now, that will be impacted by this virus in the coming weeks and the coming months.
Look, to respond to that, let me just say that the first case of coronavirus was diagnosed here in New York City in early March, so just over three weeks ago. Easter is, you know, just a couple weeks away, two to three weeks away. The idea that we can have this dramatic spike in cases — which is still going up, by the way — and that we’re somehow going to level off and be at a place where, by Easter, we’re going to have people back together again is dangerous and magical thinking. It defies all of the modeling that we’ve seen. It defies any of the reality any of my colleagues are seeing in the emergency department. And quite frankly, going into work and seeing coronavirus patients and seeing them crash and decompensating, get really sick really quickly, is scary. But this idea of millions and millions of my fellow Americans all being in church or being in concert halls or being together in just a couple weeks gives me such pause, knowing that this is the only way the virus can infect you. It cannot infect you if it cannot meet you. And by bringing people back together, this is the greatest possible risk we have to continuing and worsening this pandemic, fueling the flame across the United States.
The most important message everyone needs to know right now is the only way that you can be safe is by staying home. The virus cannot infect you if it does not meet you. The streets may look empty, I know, but I assure you what’s happening within the walls of the emergency departments here in New York City, and maybe next week in Newark and a week after that in New Mexico, it is anything but the quietness and the calm you see on those empty city streets.
AMY GOODMAN: Finally, Dr. Craig Spencer, what keeps you going? I mean, you, your colleagues, all of the health staff of all of the hospitals in this country and around the world are so incredibly brave. You are the hardest hit. What gets you to that hospital every day?
DR. CRAIG SPENCER: I just think it’s what we do. It’s our moral obligation. Yeah, we want to do it with the right equipment. Yeah, we want to do it with the right tools. But I think all of us have the sense of personal drive to be able to provide care. This is what I feel. This is what all of my colleagues have felt, all the national staff I worked with in Guinea in 2014 and 2015. I remember just being so moved by their willingness and ability to come to work every single day despite their communities being destroyed by a virus. And I’ve learned so much from them, so much that’s prepared me for this outbreak, so much that I’ve tried to share with my colleagues now.
And I think we really need to be thinking about the fact that, yes, the U.S. is really hard hit, and it’s going to get worse in the next couple weeks. But let us not forget that there is a world outside of these borders. I have worked in a lot of places where not just the critical care doctors are in short supply, but there may be no critical care beds, there may be no ventilators, there may be no ICUs or ability to provide the higher-quality care that we’re talking about right here in the United States. So, it’s just a good reminder that the media is focused so much on what’s happening in New York City, but I assure you that this is an issue and will be a greater issue everywhere else in the world. And just make sure we all keep everybody else in our thoughts.
AMY GOODMAN: Dr. Craig Spencer, I want to thank you so much for being with us, director of global health —
DR. CRAIG SPENCER: Thank you.
AMY GOODMAN: — in emergency medicine at Columbia University Medical Center, speaking to us from his home, where he also — remarkable in his work with Doctors Without Borders and many other groups, as he spends his time having been in Africa and now in New York City.
When we come back, we’ll hear the words of senator and presidential candidate Bernie Sanders on the record-shattering $2.2 trillion emergency relief bill passed by the Senate last night. Stay with us.
[break]
AMY GOODMAN: “Coronavirus Alert” by Ugandan pop star Bobi Wine and Nubian Li.










Media Options