
Topics
Guests
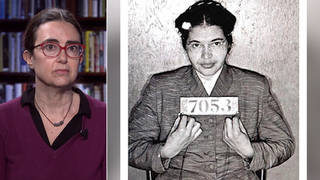
- Dr. Joia Mukherjeeinfectious disease specialist, associate professor of global health at Harvard Medical School and chief medical officer for Partners In Health, where she worked with Dr. Paul Farmer for 23 years.
We remember the life and legacy of Dr. Paul Farmer, a public health icon who spent decades building community health networks helping millions of poor people in Haiti, Rwanda, Sierra Leone and beyond. He died unexpectedly Monday at the age of 62. We feature Farmer’s past interviews with Democracy Now! and speak with his longtime colleague, Dr. Joia Mukherjee. Farmer leaves behind a remarkable legacy and an “enormous community of people that he brought to this large table that is now global health,” says Mukherjee, chief medical officer for Partners In Health, where she worked with Farmer for 23 years.
Transcript
AMY GOODMAN: “Haiti” by Arcade Fire. The Canadian band has been a big supporter of Partners In Health, having donated a portion of their ticket sales to the group for years. I was at Paul Farmer’s 50th birthday party when Arcade Fire came out and played for the celebration.
This is Democracy Now! I’m Amy Goodman, with Juan González, as we spend the rest of the hour remembering Dr. Paul Farmer. The world-renowned infectious disease doctor and medical anthropologist died unexpectedly Monday at the age of 62 in Rwanda on the grounds of a hospital and university he helped establish there. Paul Farmer was a professor at Harvard Medical School, co-founder of Partners In Health. As a medical student in 1987, he co-founded the group to deliver free, quality healthcare to people in Haiti. Over time, the group grew into an international network serving millions of patients in many of the poorest parts of the world. Dr. Farmer tirelessly fought for his patients to receive the same access to lifesaving drugs as patients in wealthy countries. Dr. Paul Farmer once said, “The idea that some lives matter less is the root of all that is wrong with the world.” Farmer’s work helped change how healthcare was delivered throughout the world.
Partners In Health CEO Sheila Davis said in a statement, quote, “Paul Farmer’s loss is devastating, but his vision for the world will live on through Partners in Health. Paul taught all those around him the power of accompaniment, love for one another, and solidarity.”
Former President Bill Clinton said Monday, “Paul Farmer changed the way health care is delivered in the most impoverished places on Earth. He saw every day as a new opportunity to teach, learn, give, and serve — and it was impossible to spend any time with him and not feel the same,” Clinton said.
The writer Tracy Kidder wrote about Farmer’s work in his 2003 book, Mountains Beyond Mountains: The Quest of Dr. Paul Farmer, a Man Who Would Cure the World.
Paul Farmer appeared on Democracy Now! numerous times over the last 20 years. Later in the show, we’ll speak with one of his longtime colleagues at Partners In Health, but first let’s turn to Paul in his own words, speaking in 2008 on Democracy Now! about his early work in Haiti.
DR. PAUL FARMER: Well, you know, it was, for me, an epiphany to go 25 years ago to go to Haiti, and I was lucky enough to end up in a squatter settlement of peasants who had lost their land to a hydroelectric dam. So the choices were very stark. You know, either health was a commodity that was bought and sold, or the people that I went there to serve, as a, you know, naive but well-meaning young person, were out of the picture. And so, you know, that began a lifelong fascination with rights, not just to the right to vote or other civil and political rights, but also the right to eat and the right to have access to healthcare.
AMY GOODMAN: Talk about how you decided on this place called Cange in central Haiti, how you found it, how you began to build the hospital system you have there?
DR. PAUL FARMER: As is often the case, and I try to encourage students — I teach students, so I tell them, “Look, you never know what’s going to happen.” And it was really a series of serendipitous accidents. I met a Haitian priest, and he was working in a nearby town, and he told me about this squatter settlement where people were living in lean-tos. And he was focused on education and said, “Look, you’re going to be a doctor. Why don’t you come and be part of this?” And so, that was 25 years ago. …
We started with a small group of young people my age going from village to village asking people in their homes, “So what is it you would see as an appropriate healthcare system?” And some people kind of laughed at us, saying, “Well, what do you” — you know, and a little but archly — “Well, what do you think?” You know, and they would usually say, though, “A hospital. We want a hospital.”
And we had in mind, you know, a system of a small community health clinic and a system of satellites. And they wanted a hospital. They wanted a good hospital, a hospital, as someone said to me in 1984, where if you have trouble having a baby, you could actually have someone save your life. I knew just what that mean, of course — meant, of course. And, you know, over the years, with a lot of help from people, mostly in Haiti, but North America, we built a hospital, and it’s a big hospital now.
AMY GOODMAN: Primarily treating what?
DR. PAUL FARMER: Well, you know, we primarily do not treat infectious diseases, although I think we have a reputation of taking on AIDS, TB, malaria. But we treat whatever comes in, a broken arm, obstructed labor, you know, the things that you see out in the rural countryside in Africa or Haiti.
But in the mid-'90s, I must say, just shortly after we built — finished — we built the hospital in a very difficult time, during a coup, and those were very hard years, ’91 to ’94. You were already involved in reporting on that. But we did get the hospital done, and by the mid-'90s, we once looked to see, OK, how many people in this hospital have AIDS or HIV infection. And it was up to 40% at one point. So we said, at that time — I was going between Harvard and Haiti. I was being trained as an infectious disease specialist at Harvard, and, you know, it’s right around the corner to Haiti. So I’d get off the plane on one side, and I’d be begging my American patients, “You’ve got to take these pills, these AIDS cocktails,” and I’d get off on the other side, and they’d be begging me for the same medicines. So we spent a couple of years saying there’s got to be a way to deliver the same services to people living in Haiti. And, you know, it took a long time to get that support. We started in 1998. And we actually called it, somewhat sassily, the HIV equity program, because we knew it would be a fight for equity from the beginning, and we knew it would be a fight for basic rights, as well.
AMY GOODMAN: And yet, you say that in some places in Haiti they’re getting better healthcare than the United States.
DR. PAUL FARMER: Well, you know, I believe that’s true. I mean, I know it’s true. It’s not really an assertion. For chronic disease — and AIDS would be a good example — you need to take — and diabetes, insulin-dependent diabetes is another — you have to take a medicine every day. You know, whether that be an antiretroviral cocktail or insulin, you have to take it every day.
And the system that we built up in the '80s, really confronting another disease, tuberculosis, relied very heavily on community health workers, who we trained and, more to the point, we paid. You know, we thought, you know, do we expropriate the labor of the poor, or do we actually pay them, like someone like I would get paid a fortune to do consulting work like this. And we said no, no, no, it's clear they have to be our employees and co-workers. So it worked great. And it worked great for tuberculosis. It worked great for other chronic diseases. And when AIDS came along, what we did was to say, well, clearly, we need to take the same system, which is free diagnosis and free care to the patient, because this is a public health problem, and they have a community health worker, you know, visiting them.
And so, what I see in this city, for example, in New York, I’m told they’re contemplating adopting this model. I hope it happens. What we did was to bring the Haiti model up to Boston. You know, and I got in a little bit of trouble with some of my colleagues. They were saying, “Well, all we’re trying to do is raise Harvard levels of care up to Haiti levels,” because the outcomes were much better, because they weren’t lost to follow-up. That’s medical jargon. But, you know, in the United States, you get someone who’s really sick with a chronic disease — either of those two diseases I mentioned, for example, would be true — and then they’re sent home, but they don’t have the appropriate support in, as they say here, in the community. And so, then they get sick again. They go back to the emergency room. Maybe they don’t have insurance, maybe they don’t speak English, maybe they have housing insecurity — this is the United States — but like Haitians, they have social problems, and our medical system doesn’t deal with those problems well. And so, the care can be better in Rwanda and Haiti than what we’re seeing here.
AMY GOODMAN: Before we get to the end of the broadcast, I want to come back here, because your analysis is not just a medical diagnosis, but it is an analysis of the healthcare system, and that’s ultimately what you’re challenging.
DR. PAUL FARMER: Well, my diagnosis of our healthcare system’s problems is that it’s very expensive to give bad medical care to poor people in a rich country, very expensive to give bad medical care to poor people in a rich country. And I can give example after example from my own clinical experience working in, you know, the best hospitals I’ve ever seen in the world. And like I said, when they’re in the hospital, things go OK. But we do not have a good safety net. We don’t have a good primary healthcare system.
And to get into the hospital, the uninsured — 47 million people, maybe 50 — they have to pass through an emergency room, waste time, and things happen to them there that probably shouldn’t, because they’re primary healthcare problems, they’re in an emergency room. And then again, on top of that 47 million, probably just as many Americans are poorly insured and can be thrown into destitution by serious illness. So, you know, there’s 100 million Americans who are in — are not — they don’t have health security. They don’t know that a devastating illness could not wipe out their savings or make them lose their home. They may know that. I hope they do.
AMY GOODMAN: That was Dr. Paul Farmer speaking in 2008 on Democracy Now! He died unexpectedly Monday at the age of 62 in Rwanda, where he lived. Today we’re remembering his life and legacy as a pioneering public health icon who spent decades building community health networks and helping millions of people in Haiti, Rwanda, Sierra Leone and other countries; joined now by one of his longtime friends and colleagues, Dr. Joia Mukherjee, infectious disease specialist, chief medical officer for Partners In Health, where she worked with Dr. Paul Farmer for 23 years. She is also an associate professor of global health at Harvard Medical School.
Joia, I want to just start off, our deepest condolences to you and to the Partners In Health family. And, of course, Paul’s family extended well beyond that — I mean, his nuclear family, but to the world, which is who he considered his family. Can you talk more about how he died, what you understand happened on the hospital grounds in Rwanda? And then talk about his significance.
DR. JOIA MUKHERJEE: Yeah. Well, first of all, Amy, thank you and the whole Democracy Now! staff for your coverage of the important issues that Paul cared about for such a long period of time and for all the condolences and wishes. And, of course, we are gutted by this loss. And, you know, I can’t really speak too much about how Paul died. You know, we’re trying to be respectful of the family, and he died peacefully. We know that. And, you know, he did have some heart trouble, which we knew about.
What it means to us is just a deep, deep sorrow, I think a sorrow for the whole world. For people who didn’t know the extraordinary man that he was, he combined a very fierce intellect with just an absolutely expansive heart and generosity and a real enthusiasm and joy for service and fellowship that was unparalleled. And at the same time, he had impossibly high standards — we all learned to live with that — high standards for medicine, that everyone should get a very First World care, that there is no First, Second and Third World, high standards for dignity. All of the hospitals that Paul was part of constructing are beautiful, have gardens and fish ponds. And he felt that, you know, there shouldn’t be squalor in healing, which is so often the case in poor communities, that the health centers and hospitals are just in deplorable condition.
But, you know, what we’re remembering today, and we will remember, is that the two things that Paul gave us were this enormous community of people that he brought to this large table that is now global health, social medicine, social justice, young people around the world who have joined this mission, you know, wealthy contributors, incredibly dedicated hospital staff, cleaners, drivers, doctors, nurses — he gave us this great community, expansive community. And the second thing he gave us — and your clip really is testament to that, Amy — is he gave us a roadmap. He was prolific in writing and speaking, incredibly clear in the idea of equity and justice for everyone. And so, I do feel grateful that we know what to do to honor his legacy: to love one another, to care for the sick, to fight for higher, fairer standards. And it’s a very radical notion, but he’s broken it down for us play by play, if you will. And I think we will honor that vision and that work by following that great roadmap.
JUAN GONZÁLEZ: And, Dr. Mukherjee, could you talk to us a little bit about how you first met him and how you came to work with him, and also about Partners In Health, which now has about 18,000 people around the world?
DR. JOIA MUKHERJEE: Yeah.
JUAN GONZÁLEZ: And how did that grow to such an extent?
DR. JOIA MUKHERJEE: Yeah. Well, you know, I came to the work in the late '90s as a very frustrated AIDS activist and doctor, having seen what Paul saw, the miracle of antiretroviral therapy and the absolute disinterest from powerful people, from the development complex, to make that treatment available to the 95% of people who were living with AIDS in the rest of the world, the large majority in Africa. And just everyone said it was too hard, it was too costly, racist things like Africans can't tell time, just a ridiculous set of narratives that I had heard in my work in Africa, before joining Partners In Health, as a young doctor, over and over again. But it wasn’t what I saw on the ground. I had incredibly intelligent friends whose lives had great meaning in their families, in their communities.
And so, I met Paul because they were treating a handful of patients in Haiti with antiretroviral therapy that was donated from patients who were changing medicine, unexpired drugs, and, you know, just saying, “At least we can do this.” I didn’t have the vision that Paul had, that this pragmatic solidarity, as he called it, could also be world-changing. Of course, now I do. And AIDS activists around the world, from ACT UP in New York to Treatment Action Campaign in South Africa to TASO in Uganda, they saw what we were doing in Haiti as a roadmap. And we started to join forces together to really call for this universal access to AIDS treatment, even though there was no universal access to healthcare at all. And so, I met him in this way. I signed up, you know, because it was the only place — Haiti was one of the only places in the world that was offering treatment for free to the destitute sick. And so, that was 23 years ago.
AMY GOODMAN: Dr. Mukherjee, I wanted to go Paul in his own words. Dr. Paul Farmer worked, as you said, in Rwanda for many years. In 2013, he appeared on Democracy Now! and spoke about his work there.
DR. PAUL FARMER: Well, you know, the work in Rwanda has been very uplifting for Partners In Health, for me, for our partners from Harvard, in part because we made a bet almost 10 years ago that if we could, as a collective, take this model — and I’ll call it accompaniment, but I’m not just talking about community-based care; I’m talking about rebuild a system that has hospitals, clinics and community-based care — if we could go to a place with great need, in terms — especially maybe in terms of infectious pathologies like malaria, TB, HIV, which we know a lot about in our team, post-conflict setting, maybe one even written off as hopeless, but with a government committed to rolling out basic services in health and education to poor people in rural areas, if we could find all that, we would see something miraculous happen in the course of a decade. And we did. That’s why we went to Rwanda. We went with the Clinton Foundation and other partners and worked with the Ministry of Health of Rwanda. And that — and it’s been the most rewarding decade in my life as a doctor just to see how — the reversal of fortune, how quickly it could happen.
Just to give you some numbers, the life expectancy in Rwanda has probably doubled over the last 10 years. And the declines in mortality, especially among children, women in childbirth, declines in mortality among those who already have tuberculosis, malaria and AIDS, these are the steepest declines ever recorded in human history. Something —
AMY GOODMAN: So explain exactly what you did.
DR. PAUL FARMER: Well, we worked with the Rwandans, as did many other people, and I’m not suggesting that, you know, we were — there are many other groups. But the key is working with the public sector. After all, eventually, if people have a right to healthcare, it will be the public sector and not nongovernmental organizations or universities from the United States that will confer those rights. So we worked to build a system. And the system stretched, as I said, from community health workers to clinics, where the majority of care is given — those are run by nurses — to having in every district a hospital. Partners In Health ended up building or rebuilding three of the 30 district hospitals, and including even starting a cancer center, probably the first cancer center in rural Africa anywhere.
But it all fit into a system, and the vertical — they’re called vertical programs in public health. So, an AIDS program or a family planning program, those are vertical programs. What the Rwandan government and authorities said is: “We want those vertical programs to strengthen our health system, our Rwandan national health system.” And we did do that. And we were pushed to do that. And the result is — I think that’s why that decline is more steeper in Rwanda than in other places and why it’s the only country in sub-Saharan Africa on track to meet all of the health-related Millennium Development goals.
AMY GOODMAN: So, that was Dr. Paul Farmer in 2013. I last “interviewed”: him in the midst of the pandemic, December 2020, when his new book, Fevers, Feuds, and Diamonds, had just come out. We talked about the pandemic, how it was possible at the time for the United States to have nearly 20% of the world’s infections and deaths, while having less than 5% of the world’s population. This was Paul’s response.
DR. PAUL FARMER: Well, I mean, we are facing the consequences of decades and decades of underinvestment in public health and of centuries of misallocation of funds away from those who need that help most. And, you know, all the social pathologies of our nation come to the fore during epidemics. And during a pandemic like this one, we’re going to be showing the rest of the world, warts and all, how — we have shown the rest of the world how badly we can do. And now we have to rally, use new tools that are coming online, but address some of the older pathologies of our care delivery system and of our country. I think that’s where we are right now.
JUAN GONZÁLEZ: That was Paul Farmer speaking about the pandemic just a couple of years ago. Dr. Mukherjee, he always referred to Partners In Health as the “House of Yes.”
DR. JOIA MUKHERJEE: Yeah.
JUAN GONZÁLEZ: What did he mean by that?
DR. JOIA MUKHERJEE: Well, I think we all know that poor people face so many barriers to having good health, I mean, starting with [inaudible] housing, lack of sanitation, water, but then even getting to the hospitals, hospitals being in deplorable conditions, not having access to modern medicine. So, I think if we are to follow Paul’s radical vision for health as a human right, which we will, the House of Yes means saying, “Yes, we can do this,” and then figuring out how and then designing a system that can do it for others.
So, you know, I’ll just talk briefly about one young man that came to an Ebola treatment unit in Sierra Leone with a giant cancer in his neck. And a normal response would be, “No, we’re treating Ebola here. Go somewhere else.” But we know there’s no somewhere else, so we said, “Yes, we will try to take care of you.” And, you know, by hook or crook, through providing chemotherapy and waiting it out and transferring him to other places, he now has graduated from high school and is completely cured of his cancer. So, you know, that House of Yes is to say we are here to care for one another on this Earth, and we’re going to try to always say “yes” and try to figure it out.
AMY GOODMAN: And so, where do you go from here, Dr. Mukherjee? What are the big projects of Partners In Health? And also, will there be a memorial service for Paul?
DR. JOIA MUKHERJEE: We are still waiting for details on the memorial service from his family. We’re in very close touch with his wife Didi and his children, and we will be working on that together.
Where we go, [inaudible] to follow the roadmap that Paul gave us. And I think, you know, he died in a place that he loved and adored, which was Rwanda, but particularly having spent time with medical students there in the new medical school that we built, the University of Global Health Equity. We are starting a second University of Global Health Equity in Haiti. And I think we know that building this vanguard of social justice and human dignity and health around the world is what he [inaudible] next and continue to do but expand the training and, you know, inculcation of these important principles.
AMY GOODMAN: Well, Dr. Joia Mukherjee, we want to thank you for being with us. Again, our deepest condolences. Dr. Mukherjee is an infectious disease specialist, chief medical officer for Partners In Health, where she worked with Dr. Paul Farmer for 23 years. She’s also an associate professor of global health at Harvard Medical School. To see all of our interviews with Paul Farmer, you can go to democracynow.org. To read about him, Tracy Kidder’s book, Mountains Beyond Mountains: The Quest of Dr. Paul Farmer, a Man Who Would Cure the World. And the Netflix film, Bending the Arc.
That does it for our show. I’m Amy Goodman, with Juan González. Stay safe.










Media Options