
Topics
A major new study of 9/11 health effects finds that nearly seven out of every ten first responders at Ground Zero suffer from chronic lung ailments. For the past five years city, state and federal officials have downplayed the health dangers of the toxic dust that was released when the World Trade Center collapsed. We speak with co-author of the Mount Sinai study. [includes rush transcript]
On September 13th, 2001–two days after the 9/11 attacks–EPA administrator Christine Todd Whitman made this announcement at Ground Zero:
- Christine Todd Whitman, 9/13/01: “Everything we’ve tested for, which includes asbestos, lead, and volatile organic compounds, have been below any level of concern for the general public health.”
Now, a major new study of 9/11 health effects finds that nearly seven out of every ten first responders at Ground Zero suffer from chronic lung ailments. The report by Mount Sinai is the largest ever done on 9/11 health effects.
For the past five years city, state and federal officials have downplayed the health dangers of the toxic dust that was released when the World Trade Center collapsed. Last week the city issued guidelines for doctors on how to spot and treat illnesses related to Ground Zero. The city was widely criticized for taking nearly five years to release the guidelines. On Tuesday, Mayor Mike Bloomberg announced the city will begin providing health treatment to anyone sickened by Ground Zero contaminants.
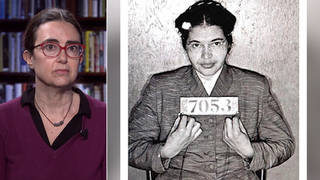
- Dr. Jacqueline Moline, co-author of the Mount Sinai study. She is the Principle Investigator and Director of the World Trade Center Monitoring & Treatment Program at Mount Sinai Medical Center.
- Lea Geronimo, one of the founders of the Beyond Ground Zero Network–an advocacy organization working with low-income and immigrant communities suffering health effects from the World Trade Center Disaster.
Transcript
JUAN GONZALEZ: On September 13th, 2001, two days after the 9/11 attacks, EPA administrator Christine Todd Whitman made this announcement at Ground Zero.
CHRISTINE TODD WHITMAN: Well, if there’s any good news out of all this, it’s that everything we’ve tested for, which includes asbestos, lead and BOCs, have been below any level of concern for the general public health.
JUAN GONZALEZ: Now, a major new study of 9/11 health effects finds that nearly seven out of every ten first responders at Ground Zero suffer from chronic lung ailments. The report by Mount Sinai is the largest ever done on 9/11 health effects.
AMY GOODMAN: For the past five years, city, state and federal officials have downplayed the health dangers of the toxic dust that was released when the World Trade Center collapsed. Last week, New York City issued guidelines for doctors on how to spot and treat illnesses related to Ground Zero. New York was widely criticized for taking nearly five years to release the guidelines. On Tuesday, Mayor Mike Bloomberg announced the city will begin providing health treatment to anyone sickened by Ground Zero contaminants.
Dr. Jacqueline Moline is coauthor of the Mount Sinai study. She’s the principal investigator and director of the World Trade Center Monitoring and Treatment Program at Mount Sinai Medical Center. Lea Geronimo also joins us, founder of the Beyond Ground Zero Network, an advocacy group working with low-income and immigrant communities suffering health effects from the World Trade Center disaster, both joining us in our Firehouse studio here in New York, just blocks from where the towers of the World Trade Center once stood. Dr. Moline, talk about the findings of your study.
DR. JACQUELINE MOLINE: Well, in the nearly 10,000 people that we report on in our study, we found that seven out of ten people had respiratory effects when they were at the site. And of those 70%, 60% still had symptoms when they were seen up to two-and-a-half years after the event. We found that half of — we found about 30% of people had abnormal breathing tests. That’s twice what we would expect in the general population.
What’s disturbing about that is, the people in our study aren’t the general population. These are people who are in physically demanding jobs, so we would assume that their pulmonary function would be better than the general population, which includes everyone in our population, so people who aren’t able to work, for example. We found that a specific breathing test of forced vital capacity, how much air you can take into your lungs, was five times more likely to be abnormal in our nonsmokers, when you compare them to the nonsmoking general population. This can explain perhaps why many of our patients feel short of breath to this day.
So the findings show that there is persistent respiratory problems, persistent upper respiratory problems and objective evidence that pulmonary function tests, standards that we followed, following every guideline, show that these problems persist. They are severe. And we’re concerned that people are going to have lasting health effects.
JUAN GONZALEZ: Now, your study involved about 9,500, or just short of 9,500 people, who were people who worked directly at Ground Zero, now? This was firefighters, police, workers on the site, as well?
DR. JACQUELINE MOLINE: The people included in our study are people who worked or volunteered at the pile, at the Fresh Kills landfill, people in the medical examiner’s office, firefighters not from New York City, because there’s a separate funding line for the FDNY, so they have an Allied program that’s also funded. These programs are funded through the National Institute for Occupational Safety and Health. So, police officers, construction workers, clergy, volunteers of all sorts.
AMY GOODMAN: And when you say Fresh Kills, for people not from here, you mean in Staten Island at the dump.
DR. JACQUELINE MOLINE: Right, where they brought all the debris. They sifted through the debris. So people there had similar exposures, because everything there was dusty as well.
JUAN GONZALEZ: And in terms of the — your expectation is that many of these people may have to be treated for the rest of their lives to some extent or could be suffering effects for the rest of their lives?
DR. JACQUELINE MOLINE: This study reports through 2004. We’ve continued with the medical monitoring program and our treatment programs to see people who worked or volunteered at the site. And these people are still sick. And we’re at the five-year anniversary now. And we can assume that people who have chronic ailments, these problems aren’t going away. And it’s likely that they will need ongoing treatment.
AMY GOODMAN: Chronic ailments, like what?
DR. JACQUELINE MOLINE: Like asthma, like chronic rhinosinusitis, irritation of the sinuses and the nose, chronic cough, chronic throat irritation. Our study doesn’t report on the mental health findings, which will be coming out in the next few months. But we know that many of our participants have some severe mental health problems that result from their exposures down there: post-traumatic stress disorder, anxiety, panic attacks, generalized depression. So, these are all lifelong, potentially lifelong problems.
And then, of course, we’re concerned about the future for many of our patients. We don’t know what’s going to happen in the future, and we’re concerned there are some cases where patients have lung scarring, you know, that we’re right at the cusp of when we would expect to see a lot of these diseases start. The interstitial fibrosis, the medical term for lung scarring, for example, five years is really when you start to see it. We’ve seen it actually a little earlier in some patients. But is the next wave going to happen in the next few years? And that’s why it’s essential to continue the funding for these programs, which actually runs out in 2009.
AMY GOODMAN: Dr. Moline is with Mount Sinai. She is running the study that looks at what has happened to the first responders now, five years later. We’re also joined by Lea Geronimo, who is one of the founders of Beyond Ground Zero Network. Dr. Moline is talking about the rescuers, the first responders. Talk about who you represent.
LEA GERONIMO: Actually, I am a resident of the Lower East Side for almost six years, and I’ve worked on Wall Street for about ten. So, clearly, the week after the tragedy, many of my co-workers and I were expected to come back to work the very next week, when it wasn’t clean, the fires were still burning for a year and a half. So there’s a re-ignition of fires that were happening.
AMY GOODMAN: On September 11th, where were you?
LEA GERONIMO: I was lucky to be in my apartment, but I was still downtown. I live on 13th Street, so I was still below the 14th Street cutoff. I came to work. I had been exposed to all the fires. Within the first few months, I was experiencing heavy menstrual bleeding for almost six months. I started to develop bronchitis and now have become — now this problem has become chronic. I’ve had it nine times since 9/11. I’ve also had psoriasis since I was young, but just little patches maybe on my scalp, and now it’s to the point where I have it on my thighs, my back, my scalp. You can see a little spot here on my elbow. I’ve had to go to my dermatologist three times a week to get UV light treatments, as well as use various different topical creams.
And I was relatively healthy. I’m a 35-year-old pretty young person that didn’t have any significant health problems before 9/11. And I’m one of many people who have been forgotten, because many residents, as well as other workers, such as office workers in the downtown area, have no programming to go to, with the exception of the program that’s at Bellevue, which is sort of the sister program to Mount Sinai. Unfortunately, our program has not been funded by the government, so it is very hard and a long wait for a lot of the undocumented population that are not being seen at Mount Sinai, as well as residents and other workers who worked downtown but are not cleanup workers.
JUAN GONZALEZ: Well, Mayor Bloomberg actually made an extraordinary announcement on the same day that your report came out, the Mount Sinai report, which is a little questionable in my mind, the timing of his announcement at the same time that the Mount Sinai report was coming out. But the Mayor announced that the city will now begin to fund health treatment at Bellevue for anyone who believes that they are sick as a result of 9/11 exposure, so that would include residents. It would include office workers. And he specifically said that the city’s policy is not to deny treatment to anybody because of their immigration status. But the question is, of course, what the cost this will be to the city on a long-term basis. And he’s trying now to see about federal funding.
What’s your perspective on this whole issue of the federal government’s responsibility in assuring that people do not continue to be exposed, because in some of these buildings, because the city allowed owners to self-certify their cleaning, no one really knows how decontaminated some of these buildings are?
LEA GERONIMO: Well, there’s still the old Deutsche Bank building that’s still up, which has, from my understanding, toxins that are a hundred times stronger than what was released at 9/11. So there are still toxins in the area. I don’t know how easy this is going to be, since the cleanup wasn’t done sufficiently from the beginning. I’m also concerned that there are a lot of people, who because their doctors weren’t given, until recently, this list by the New York City Department of Health of symptoms of 9/11 diseases, that they weren’t being recognized and connected. And a lot of people who do see doctors outside of Manhattan, you know, the other five boroughs, you know, they were having a very hard time getting their doctors connecting all of these problems. So we have the two problems. We have the cleanup, and we will have the health of people who aren’t even considered part of the affected group.
JUAN GONZALEZ: And, Dr. Moline, your project is basically a monitoring program. Does it also do treatment? And what percentage of the workers that you’ve been dealing with have health insurance to be able to deal with some of these problems?
DR. JACQUELINE MOLINE: Well, we have — the initial funding was purely for monitoring, and it was actually a screening program that has morphed into a monitoring program, as we’re seeing people for repeat evaluations. Initially we received money for treatment from philanthropic sources, the generosity of the Bear Stearns Charitable Trust, the 9/11 Fund, New York Community Trust, a number of other charitable organizations, and then the American Red Cross, who has stepped up and has provided funding for both Mount Sinai, other clinics including Bellevue, to see —- for their limited program now that will be expanded now through federal funding. We recently -—
AMY GOODMAN: I didn’t hear you say federal government in that.
DR. JACQUELINE MOLINE: I’m just about to add that. The federal government is providing treatment monies, most of it will be forthcoming in the next few months. It was from the $125 million reappropriation that was taken out of the President’s budget, and then through the work of the New York Congressional delegation really and the work of organized labor in getting this funding back —
AMY GOODMAN: But for five years, you didn’t have federal funding?
DR. JACQUELINE MOLINE: For five years we did not have federal funding for treatment.
AMY GOODMAN: For dealing with police, for example, who were suffering after the attacks.
DR. JACQUELINE MOLINE: We didn’t have any federal funding for treatment at all. We now will have some. We’re waiting for it to come in. The money isn’t adequate, certainly. We know that medical treatment costs are high.
In our treatment program, 38% of the people in our treatment program have no health insurance. 42% are underinsured. Only 20% have full, full coverage. So what we’re finding is that, while there’s the Workers’ Compensation system, which although these people have work-related problems, the system is difficult to navigate for anybody. And many of these people have had Workers’ Comp claims that have been controverted, or they’ve been disputed, so there’s delays in getting treatment. Once they do have a case, there may be delays in getting treatments authorized. So it’s been a very difficult road for many of these patients.
And the treatment program luckily, through the generosity of philanthropy, frankly, has been able to bridge that gap and provide treatment to people. We actually have seen many immigrants, day laborers, in the monitoring and treatment programs that are available, besides the Bellevue program. We have about 14% of our population in the screening program, English is not their first language. We have a large immigrant population within the monitoring program, and that’s reflective of who worked down at the site. So many of the building cleaners, for example, the laborers, they are immigrant workers that we have been proud to be able to monitor and treat.
AMY GOODMAN: And finally, Lea, can you talk about how race and class fits into this?
LEA GERONIMO: Well, for me, I’m not sure if I see it on that level exactly, because there were all kinds of people from different ethic graphic groups that have been excluded. There have been all kinds of people from different class levels that have been excluded, because I think, one, the government is just recently saying that the air is toxic, finally. So that’s one problem. And two, there was no bubble over the area. It didn’t matter if you were rich. It didn’t matter if you were from a certain group. You were affected.
And getting back to what you were saying about that $125 million, part of the problem was when that money came from the federal government to the state, people were blocked out of those cases, because either they had surpassed the two-year statute of limitations or they were undocumented. And then, the government’s saying, well, you know, this is a surplus, so let’s just give it back. But really what it did is it set up parameters that excluded residents from getting the money, it excluded undocumented population from getting the money. So in that respect, yes, there was definitely exclusions.
AMY GOODMAN: So they didn’t ask for their papers when they were cleaning, but now ask for their papers when they’re sick.
LEA GERONIMO: Exactly.
AMY GOODMAN: I want to thank you both for being with us: Dr. Jacqueline Moline, vice chair of the Mount Sinai Medical Center Department of Community and Preventive Medicine, she is principal investigator and director of the World Trade Center Monitoring and Treatment Program at Mount Sinai; and Lea Geronimo, one of the founders of the Beyond Ground Zero Network, an advocacy group working with low-income and immigrant communities suffering from the health effects at the World Trade Center disaster. Thanks for joining us.
[break]
AMY GOODMAN: Before we move on to our next segment, Juan, you’re going to be chairing a major town hall meeting tonight in New York around Ground Zero, is that right?
JUAN GONZALEZ: Yes, I’m going to be moderating a town hall meeting at St. Paul’s Church in the Financial District, where many of the medical experts, as well as residents and others, will be addressing what’s happened five years later in terms of the health of folks. And, you know, it’s very interesting now, you’re getting all of this media coverage. The New York Times has produced a Ground Zero film that’s on the Discovery Channel. CBS News has produced a Ground Zero film that will be on the Sundance Channel. And there are all of these articles now about the terrible health effects of people. But five years ago, you know, the New York Times did almost virtually nothing. In fact, basically bought hook, line and sinker the EPA and the city’s position on this issue and did very little coverage of the health effects, and so I —
AMY GOODMAN: You were really pioneering in that. I mean, you then ended up writing the book Fallout precisely about this issue.
JUAN GONZALEZ: Right, precisely about this. And back then, there was enormous outcry from the business community, from the Mayor’s office, from the EPA, about anybody questioning their results. And I keep wondering, all of these media that are now on a bandwagon of “let’s do something about the health of all the people,” where were they when they were really needed by the public five years ago to question the government’s role in all of this?
AMY GOODMAN: Well, of course, we’ll continue to cover this, as we move into this fifth anniversary of 9/11.










Media Options